Coronary physiology is the collective term for a group of indexes aimed at directly measuring the intracoronary haemodynamic changes that occur across a stenosis in order to guide revascularisation decision-making. Fractional flow reserve (FFR) uses pharmacological dilatation and miniaturised pressure-wires to measure coronary pressure proximal and distal to a stenosis, thereby estimating flow reduction across a stenosis. Several clinical trials have shown that FFR-guided revascularisation improves clinical outcomes, and that deferring revascularisation in patients shown by FFR to have non-haemodynamically significant lesions is safe. Instantaneous wave-free ratio (iFR) is a novel technique that measures the ratio of distal coronary to aortic pressure during a specific period in diastole that obviates the need for pharmacological vasodilatation. Recent randomised-controlled trials have shown iFR to be non-inferior to FFR with respect to major adverse cardiac events, while reducing adverse procedural symptoms and procedure duration.
Introduction – why do we need coronary physiology?
It is increasingly appreciated that only coronary stenoses severe enough to cause myocardial ischaemia should undergo revascularisation. Reliable assessment of stenosis severity is, therefore, vital. For many years, invasive coronary angiography was considered to be the gold-standard test for the identification of flow-limiting coronary artery disease. This was largely due to the ‘oculo-stenotic reflex’ – a powerful stimulus that leads operators to believe that ischaemia must be present based on the severity of the coronary stenosis from visual assessment alone. However, identifying ischaemia using only a two-dimensional angiographic image grossly oversimplifies the relationship between a stenosed vessel (a complex three-dimensional structure) and the relevant area of subtended myocardium it supplies.
Since the pioneering work of Andreas Grüntzig in the late 1970s,1 efforts have been made to objectively quantify the haemodynamic impact of a stenosis, thereby circumventing many of the limitations of a visual-based approach to revascularisation decision-making. The approach of directly measuring intracoronary haemodynamic changes that occur across a stenosis is collectively termed ‘coronary physiology’. Following years of development (and the necessary miniaturisation of pressure-wire sensor technology), coronary physiology-guided revascularisation is now a well-established tool in the modern management of patients with stable coronary artery disease.
In this article, we review the scientific principles and key clinical outcome studies behind the two most commonly used coronary physiology indexes – the fractional flow reserve (FFR) and the instantaneous wave-free ratio (iFR). We also include instructional figures describing how to perform high-quality FFR/iFR measurements in routine clinical practice.
Fractional flow reserve
Basic principles
Myocardial ischaemia is a flow-based pathology. However, performing measurements of intracoronary flow is technically difficult and is, thus, largely confined to research settings. Attention has, therefore, turned to measuring intracoronary pressure (which is technically much simpler to measure), as a clinically applicable surrogate measure of flow. The basic principle of FFR is to eliminate the resistance of the microcirculation using pharmacological dilatation. This is termed maximal hyperaemia. Analogous to Ohm’s law (V=IR, where V is voltage difference, I is current and R is resistance), it can be assumed that when coronary resistance is stable and minimal (as occurs during maximal hyperaemia), a direct relationship exists between coronary pressure and flow. As such, in the context of hyperaemia, coronary pressure measurements can be used to assess the functional impact of a stenosis on the myocardium.
In 1993, Pijls et al.2 introduced FFR as a means of determining coronary flow using pressure-only-based assessments during hyperaemia. FFR is defined as the ratio of the pressure distal to a stenosis (Pd) relative to the pressure proximal to the stenosis (Pa) during maximal hyperaemia. As such, a FFR value of 0.80 represents a pressure loss across the stenosis of 20%.
FFR clinical outcome studies
Since its introduction, several studies have explored the clinical outcomes of patients whose revascularisation decision-making was guided by using FFR (table 1). The DEFER (Deferral Versus Performance of PTCA in Patients Without Documented Ischemia) study randomised 325 patients with stable coronary disease to one of three groups. Patients with a FFR ≥0.75 were randomly assigned to deferral or angioplasty, while those with a FFR <0.75 underwent angioplasty as planned.3 Originally reported outcomes at 24 months, in addition to longer-term follow-up at five and 15 years,4,5 showed that in patients with stable coronary disease, deferring revascularisation of a stenosis with a FFR ≥0.75 is comparatively safe and that revascularisation conferred no additional therapeutic benefit.

The subsequent FAME study (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) assessed the clinical effectiveness of FFR-guided versus angiography-guided revascularisation of patients with multi-vessel coronary artery disease.6 One thousand and five patients with at least a 50% stenosis in two major epicardial arteries were randomised to undergo revascularisation using drug-eluting stents guided by angiography alone or FFR measurements. It should be noted that the FAME study used a higher FFR value of 0.80 as the clinical cut-off value for functionally significant lesions in an attempt to decrease the number of ischaemic lesions left untreated. The results of the FAME study showed that routine use of FFR-guided revascularisation in multi-vessel coronary artery disease was associated with a significant reduction in major cardiac adverse events (MACE) at one year compared with angiography alone.
The FAME 2 study7 built on these previous works by comparing FFR-guided percutaneous coronary intervention (PCI) plus optimal medical therapy (OMT). In this study, 1,220 patients with multi-vessel coronary artery disease had all stenoses visible on angiography measured using FFR. Patients with at least one stenosis with a FFR ≤0.8 underwent randomisation to either receive FFR-guided PCI plus OMT or OMT alone. Patients in whom all stenoses had a FFR >0.80 received OMT. The primary end point was a composite of death, myocardial infarction (MI) or urgent revascularisation. The study was halted prematurely due to a significant reduction in the composite primary end point in the PCI group. However, as this was driven by significantly fewer urgent revascularisations (in an unblinded study design), rather than decreased mortality or MI, the FAME 2 authors had to limit their conclusions to FFR-guided PCI plus OMT results in decreased rates or urgent revascularisation compared with OMT alone.
Instantaneous wave-free ratio
Basic principles
iFR was first invented in 2012 and has grown rapidly as a physiological index to guide revascularisation decision-making. Like FFR, iFR utilises intracoronary pressure to provide an estimation of intracoronary flow. However, unlike FFR, iFR achieves this task without requirement for pharmacological vasodilatation. This is because iFR measures the ratio of distal coronary to aortic pressure during a period in diastole where microvascular resistance is naturally at its most stable. By only measuring pressure within this specific portion of the cardiac cycle, iFR facilitates the pressure-only assessment of the haemodynamic impact of a coronary stenosis without the need for pharmacological vasodilatation.
iFR clinical outcome studies
Recent clinical outcome studies have addressed the safety of using an iFR-alone versus FFR-alone approach to guide revascularisation decision-making (table 2). The DEFINE-FLAIR (Functional Lesion Assessment of Intermediate Stenosis to Guide Revascularisation)8 and the iFR-SWEDEHEART (Instantaneous Wave-Free Ratio Versus Fractional Flow Reserve in Patients With Stable Angina Pectoris or Acute Coronary Syndrome Trial)9 trials randomised patients with coronary stenosis of intermediate severity to undergo either FFR-guided or iFR-guided revascularisation, using cut-off values for FFR and iFR of 0.8 and 0.89, respectively. Both trials included stable angina patients and also those with acute coronary syndrome (ACS) with non-culprit intermediate disease and are the largest coronary physiology trials ever conducted.

The primary results of DEFINE-FLAIR and iFR-SWEDEHEART demonstrated that iFR-guided revascularisation was non-inferior to FFR with respect to MACE at one year. In addition, several secondary outcomes favoured iFR. Both trials showed over a 10-fold reduction in adverse procedural symptoms in the iFR group compared with the FFR group, as well as shorter duration of procedure. Furthermore, a meta-analysis of the DEFINE-FLAIR and iFR-SWEDEHEART studies also revealed that significantly less myocardial revascularisation (by either PCI or coronary artery bypass graft [CABG]) was performed when iFR was used.10
Following these landmark trials, the most recent European Society of Cardiology (ESC) guidelines have granted iFR a class 1A recommendation in assessing the haemodynamic relevance of intermediate-grade stenoses.11
iFR pullback – the future of coronary physiological assessment?
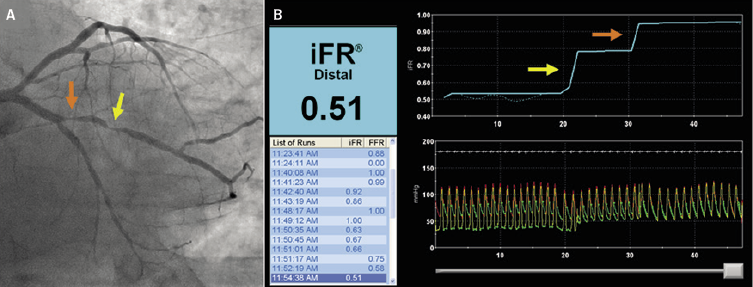
An important advantage of iFR over FFR is in the evaluation of coronary arteries in which there are serial stenoses, i.e. two or more lesions within the same coronary vessel. In serial stenoses, physiological assessment with FFR is confounded by the cross-communication that exists between stenoses under hyperaemia. In this situation, hyperaemic flow through one stenosis is limited by the presence of another stenosis and vice versa. However, because resting coronary flow remains stable across almost the entire range of stenosis severities, resting assessment of pressure changes using iFR allows isolated assessment of an individual stenosis, even when in series.12 By measuring continuously during a manual pressure-wire pullback, iFR pullback is able to map and quantify the haemodynamic significance of each individual stenosis, as well as allowing operators to predict the physiological benefits of revascularisation – so called ‘virtual PCI’ (figure 1).13
How to perform a pressure-wire assessment?
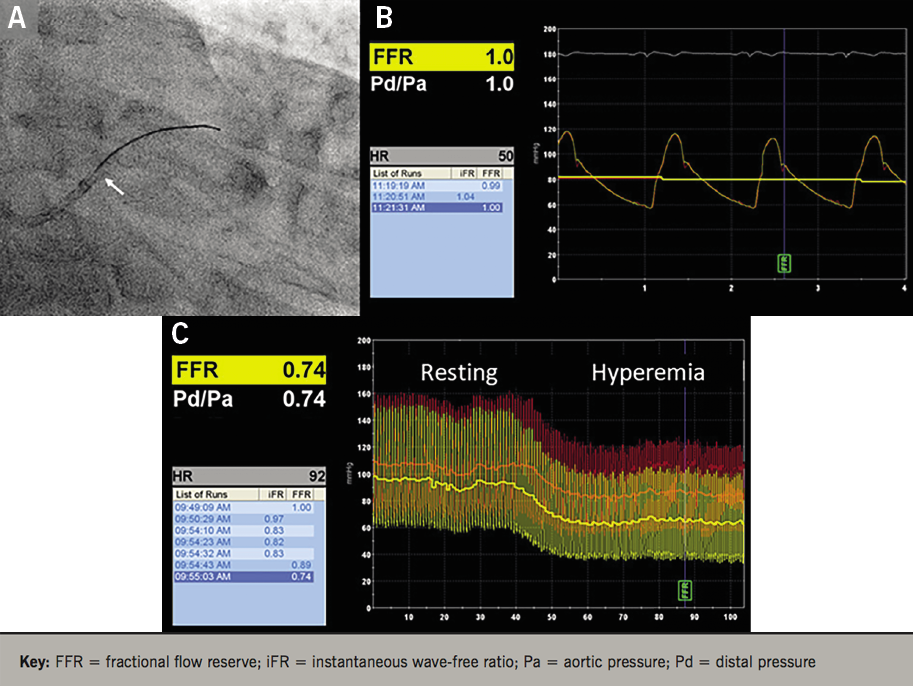
Regardless of the choice of physiological index used to guide revascularisation decision-making, reproducible high-quality measurements are essential to ensure that accurate FFR or iFR measurements are obtained (figure 2). After diagnostic angiography, a sensor guidewire is passed through an angioplasty Y-connector attached to a diagnostic or guiding catheter. Heparin and nitroglycerin are then given to minimise vasomotion, ensuring high-quality and accurate measurements. After calibration against atmospheric pressure, the sensor-wire is then introduced into the patient and positioned at the tip of the guiding catheter, thereby enabling the pressure in the aorta and that recorded by the pressure-wire transducer to be equalised (figure 3). The wire is then advanced across the stenosis and, when performing FFR, a pharmacological hyperaemic stimulus (usually adenosine) is then administered. At peak hyperaemia, the FFR is calculated as the ratio between the mean distal coronary pressure (measured by the pressure wire) and mean aortic pressure (measured by the guiding catheter).14

Conclusion
Coronary physiology-guided revascularisation with either FFR or iFR represents contemporary gold-standard practice for the invasive management of patients with intermediate severity coronary artery disease. Recent clinical trials support the use of iFR alone, particularly in guiding revascularisation of tandem lesions.
While current treatment guidelines interpret the results of coronary physiology in a binary fashion (i.e. FFR ≤0.80 ‘ischaemic’ versus FFR >0.80 ‘non-ischaemic’), it should always be remembered that ischaemia is in fact a continuum of disease. As such, revascularisation decisions, particularly when coronary physiology measurements are borderline, should always be interpreted on an individual patient basis utilising all of the available clinical information.
Key messages
- Visual assessment by traditional coronary angiography is unable to distinguish whether a coronary stenosis is haemodynamically significant, particularly in intermediate severity coronary artery disease
- Coronary physiology-guided revascularisation with either fractional flow reserve (FFR) or instantaneous wave-free ratio (iFR) is able to directly measure intracoronary haemodynamic changes in order to guide revascularisation decision-making
- FFR uses pharmacological vasodilatation to eliminate microvascular resistance and is defined as the ratio of the pressure distal to a stenosis (Pd) relative to the pressure proximal to the stenosis (Pa) during hyperaemia
- iFR measures the ratio of distal coronary to aortic pressure during a specific period in diastole where microvascular resistance is at its most stable, thereby eliminating the need for pharmacological vasodilatation
- Regardless of the choice of physiological index used to guide revascularisation decision-making, high-quality, reproducible measurements are essential to ensure accurate FFR or iFR measurements are obtained
Conflicts of interest
MS none declared; CC and TW have received consulting fees from Philips; JD holds patents pertaining to the iFR technology. JD is a consultant for Philips Volcano and has received research grants from Philips Volcano.
References
1. Grüntzig AR, Senning A, Siegenthaler WE. Nonoperative dilatation of coronary-artery stenosis: percutaneous transluminal coronary angioplasty. N Engl J Med 1979;301:61–8. https://doi.org/10.1056/NEJM197907123010201
2. Pijls NHJ, van Son JAM, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation 1993;87:1354–67. https://doi.org/10.1161/01.CIR.87.4.1354
3. Bech GJW, De Bruyne B, Pijls NHJ et al. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation 2001;103:2928–34. https://doi.org/10.1161/01.CIR.103.24.2928
4. Pijls NHJ, van Schaardenburgh P, Manoharan G et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER study. J Am Coll Cardiol 2007;49:2105–11. https://doi.org/10.1016/j.jacc.2007.01.087
5. Zimmermann FM, Ferrara A, Johnson NP et al. Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. Eur Heart J 2015;36:3182–8. https://doi.org/10.1093/eurheartj/ehv452
6. Tonino PAL, De Bruyne B, Pijls NHJ et al.; FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 2009;360:213–24. https://doi.org/10.1056/NEJMoa0807611
7. De Bruyne B, Pijls NHJ, Kalesan B et al.; FAME 2 Trial Investigators. Fractional flow reserve–guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991–1001. https://doi.org/10.1056/NEJMoa1205361
8. Davies JE, Sen S, Dehbi HM et al. Use of the instantaneous wave-free ratio or fractional flow reserve in PCI. N Engl J Med 2017;376:1824–34. https://doi.org/10.1056/NEJMoa1700445
9. Götberg M, Christiansen EH, Gudmundsdottir IJ et al.; iFR SWEDEHEART Investigators. Instantaneous wave-free ratio versus fractional flow reserve to guide PCI. N Engl J Med 2017;376:1813–23. https://doi.org/10.1056/NEJMoa1616540
10. Escaned J. Safety of coronary revascularisation deferral based on iFR and FFR measurements in stable angina and acute coronary syndromes. Presented at EuroPCR 2017 on 1 May 2017 in Paris, France. Available from: https://solaci.org/_files/PCR2017/EscanedJavier.pdf
11. Neumann FJ, Sousa-Uva M, Ahlsson A et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 2018;40:87–165. https://doi.org/10.1093/eurheartj/ehy394
12. Nijjer SS, Sen S, Petraco R et al. Preangioplasty instantaneous wave-free ratio pullback provides virtual intervention and predicts hemodynamic outcome for serial lesions and diffuse coronary artery disease. JACC Cardiovasc Interv 2014;7:1386–96. https://doi.org/10.1016/j.jcin.2014.06.015
13. Kikuta Y, Cook CM, Sharp ASP et al. Pre-angioplasty instantaneous wave-free ratio pullback predicts hemodynamic outcome in humans with coronary artery disease: primary results of the international multicenter iFR GRADIENT registry. JACC Cardiovasc Interv 2018;11:757–67. https://doi.org/10.1016/j.jcin.2018.03.005
14. Kern MJ, Lerman A, Bech JW et al. Physiological assessment of coronary artery disease in the cardiac catheterization laboratory: a scientific statement from the American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology. Circulation 2006;114:1321–41. https://doi.org/10.1161/CIRCULATIONAHA.106.177276
