Radial artery access coronary angiography is associated with high procedural success and lower rates of complications, compared with femoral access, in patients without prior coronary artery bypass surgery (CABG). Whether or not this applies to patients who have undergone CABG is not known.
We retrospectively examined hospital records of 5,993 consecutive patients undergoing coronary angiography to identify patients with previous CABG undergoing the procedure by the radial or femoral access routes. We compared clinical characteristics, procedural success and complications up to 30 days, adjusting for significant baseline differences.
Among the 5,993 patients undergoing angiography, 471 (8%) had previous CABG; 164 (35%) underwent angiography by the radial and 307 (65%) by the femoral artery. Procedural success was lower in the radial than femoral groups; 28/164 (17%) radial versus 1/307 (0.3%) femoral patients required access-site cross-over (p<0.001) and 254/347 (73%) versus 496/594 (84%) bypass grafts were selectively identified without the need for further imaging investigations (p=0.008), respectively. Access-site bleeding requiring compression affected 1/164 (0.6%) in the radial group and 12/307 (3.9%) in the femoral group (p=0.04 for difference) with no significant differences in other major complications.
About one in 12 patients undergoing coronary angiography have had previous CABG surgery. In such patients, the radial access route was associated with lower procedural success than the femoral route but also a lower rate of bleeding complications.
Introduction
Invasive coronary angiography is the definitive diagnostic test for assessing coronary artery patency.1 For many years, the femoral artery was the usual vascular access site for such procedures, but use of the radial artery has increased due to it being more superficial and easier to compress following the procedure. In the UK, the radial artery was used in about 10% of all coronary angiograms in 2004, and this steadily increased to 84% by 2016.2 Advantages of the radial approach include better haemostasis,3,4 earlier ambulation and increased patient satisfaction.5,6 Randomised trials comparing radial access coronary angiography with femoral access coronary angiography have demonstrated reduced rates of vascular complications using radial access, without compromising procedural success.5,7-11
Coronary angiography in patients with previous coronary artery bypass surgery (CABG) is complicated by the need to assess the patency of bypass grafts, as well as the coronary arteries.12 Such patients were excluded from the randomised trials comparing radial with femoral access angiography, leaving uncertainty over the preferred vascular access route in this subset of patients.
This prompted us to examine the outcomes of consecutive patients with previous CABG undergoing diagnostic coronary angiography by the radial or femoral vascular access routes and to compare procedural success and clinical outcomes at 30 days.
Materials and method
We used electronic hospital coding data to identify patients who had undergone coronary angiography over a one-year period at St. Bartholomew’s Hospital, a tertiary cardiac centre in London, UK, that receives elective and emergency referrals from eight other hospitals. Hospital records were examined to identify patients with previous CABG. Clinical and angiographic characteristics were determined from the procedure reports and, in cases where these data were incomplete, from review of the angiograms. Clinical outcomes following angiography, including bleeding (minor, requiring arterial compression and major, requiring blood transfusion or vascular repair), stroke, myocardial infarction, hospitalisation for renal or heart failure, and death up to 30 days following the procedure, were determined by clinical record review at the heart centre and referring hospitals. Patient management, including the decision to use the radial or femoral vascular access route for coronary angiography together with decision to proceed to immediate percutaneous coronary intervention (PCI) and the use of vascular compression or closure devices following the procedure, were at the clinical discretion of the supervising cardiologist.
Procedural success was assessed as the number of patients requiring access-site cross-over and the number of grafts selectively identified by cardiac catheterisation before additional imaging was required. Patients with bilateral internal mammary grafts and those undergoing planned elective PCI, where the vascular access route had been pre-determined from a previous angiogram, were excluded.
Patients in the radial and femoral access groups were compared in terms of clinical characteristics and angiographic and clinical outcomes. Binary variables were reported as absolute numbers and percentages and continuous variables were reported as median and interquartile range where they did not fit a Gaussian distribution, or mean and standard deviation where they did. Comparisons between the radial and femoral access groups were made using Fisher’s exact test for binary variables or using the Wilcoxon rank-sum test or t-test, as appropriate, for continuous variables. Logistic regression was used to adjust for the effect on clinical outcomes of any significant differences in baseline characteristics. All analyses were performed using Stata version 14 (StataCorp, College Station, Texas).
Results
Among 5,993 patients undergoing coronary angiography between September 2016 and September 2017, 471 (8%) had previous CABG; 164 (35%) undergoing angiography by the radial artery and 307 (65%) by the femoral artery. The clinical characteristics of the two groups are shown in table 1. A history of smoking and myocardial infarction was more common in the femoral compared with the radial group. Graft notes, detailing the number and location of bypass grafts previously implanted, were missing in 23% of patients (mostly emergency patients). Among patients in whom graft notes were available, there were 299 grafts with a subclavian origin (289 left and 10 right internal mammary arteries) and 642 with an aortic origin (all saphenous veins); with no significant difference between the radial and femoral groups. Table 2 gives the angiographic details according to vascular access site. Fluoroscopy time was 18 minutes in the radial access group and 15 minutes in the femoral access group (p=0.045 for difference). One hundred and six radial procedures were from the left arm versus 57 from the right arm (no right-arm patients had a left internal mammary graft). Two hundred and eighty-four femoral procedures were from the right leg and 22 from the left leg.
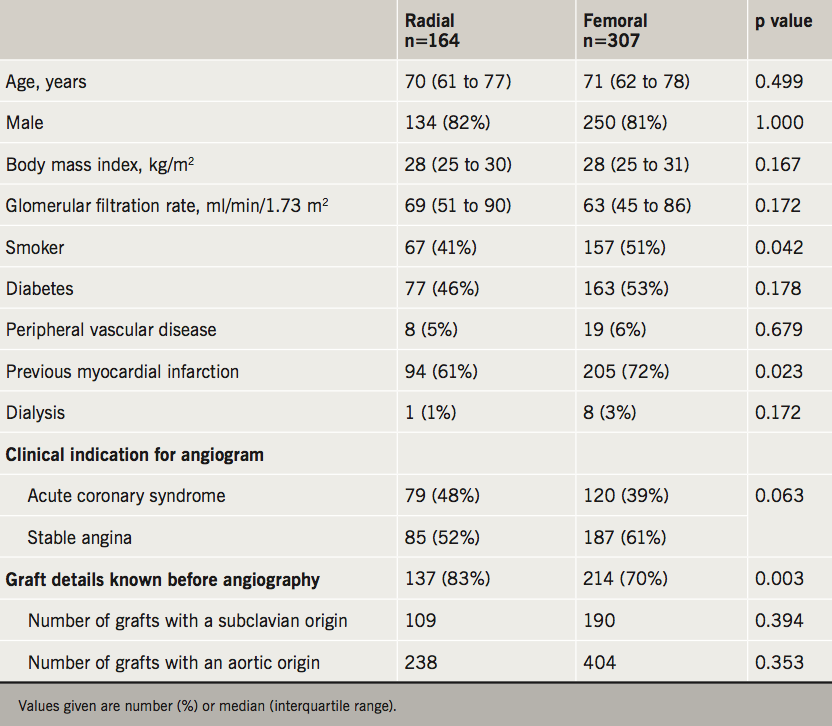
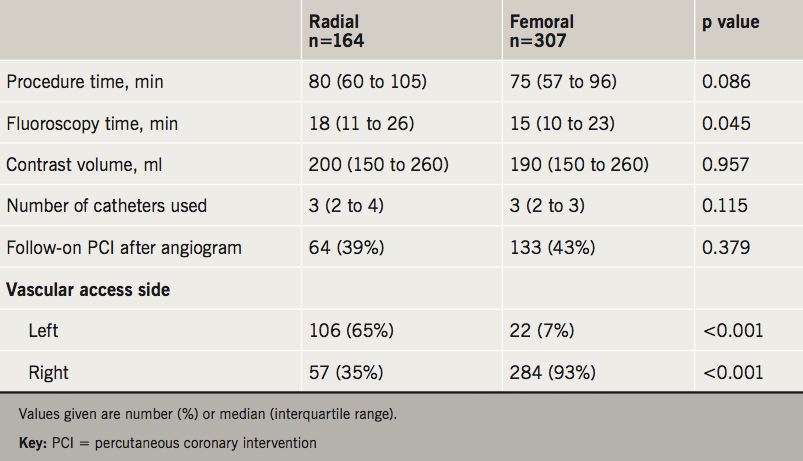

Figure 1 shows procedural success in the radial and femoral groups; (a) the number and proportion of patients who required access-site cross-over because of a failure to complete the procedure by the initial access route – 28/164 (17%) and 1/307 (0.3%), respectively (p<0.001), and (b) the number and proportion of bypass grafts that were successfully identified without the need for other imaging investigations – 254/347 (73%) and 496/594 (84%), respectively (p=0.008). Patients in whom grafts were not identified during the initial angiogram went on to have computed tomography (CT) coronary angiography or repeat invasive angiography.
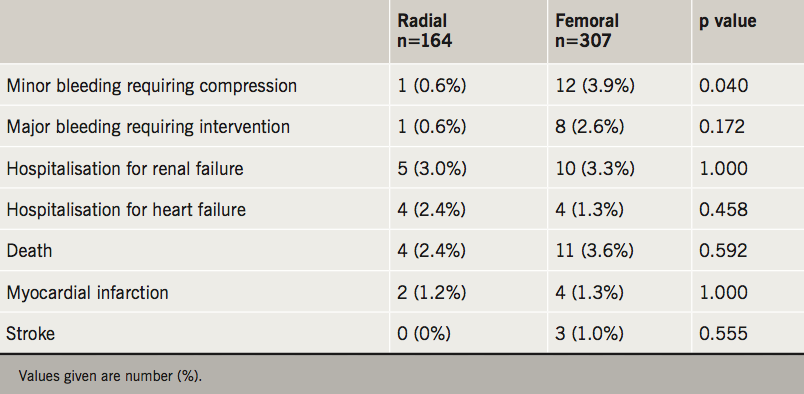
Table 3 shows the clinical outcomes up to 30 days post-procedure according to vascular access site. Minor access-site bleeding requiring compression affected 1/164 (0.6%) in the radial group and 12/307 (3.9%) in the femoral group (p=0.04 for difference), with no significant differences in major complications including major bleeding, myocardial infarction, heart or renal failure, stroke or death between the two groups. Sequential adjustment for baseline differences between the two groups did not alter these results.
Discussion
Our results indicate that coronary angiography in patients with previous CABG is associated with higher rates of procedural success using the femoral compared with the radial vascular access route with an increase in bleeding needing compression, but not in major clinical complications.
The finding that access-site bleeding was greater in the femoral than radial group is consistent with randomised trials comparing radial with femoral access angiography.13,14 Patients with previous CABG were not, however, included in these trials because of concerns over technical complexity and procedural success, leaving uncertainty over whether the net advantages of radial vascular access can be similarly applied to patients with previous CABG. Our results indicate that procedural success was lower with the radial approach, both in terms of selective cannulation of bypass grafts and the need for access-site cross-over. The higher position of the aortovenous anastomoses of saphenous vein grafts in the ascending aorta makes a Judkins right catheter curve or graft-seeking catheters less suited to selective cannulation of bypass grafts from the left radial, which may explain this result.
Three previous studies have compared radial with femoral angiography in CABG patients, but they assessed procedural success only in terms of the need for access-site cross-over. One study with 304 patients observed a 4% radial to femoral cross-over rate versus 1.3% for femoral to radial,15 another study with 404 patients observed 3% versus 0%,16 and in a third study with 124 patients, it was 1% versus 0%, respectively.17 It is not clear why the cross-over rate observed in our series (17% versus 0.3%) was higher than in these earlier reports but our result is consistent with the only randomised trial (128 patients) conducted to date,18 which showed access-site cross-over rates in the radial and femoral groups of 17% and 0%, respectively.
Limitations
The main limitation of our study was its non-randomised design, making it susceptible to selection bias. Apart from a higher rate of smoking and previous myocardial infarction in the femoral group, which would tend to favour the radial group outcomes, the two groups were well matched in baseline characteristics, including body mass index, diabetes, renal function and peripheral vascular disease. Adjustment for baseline differences did not affect the results, but the possibility of confounding by unknown factors remains. The statistically significant increase in minor bleeding and the trend towards an increase in major bleeding complications in the femoral group highlights the need for an adequately powered randomised trial, limited to patients with previous CABG, to provide definitive evidence of benefit of one access route over the other. About 80% of coronary angiograms in our service are radial access procedures, so any observed advantage of femoral over radial is unlikely to be due to inexperience. This is, however, a single-centre study, so the results may not be generalisable, but may prompt similar audits of outcomes in other centres.
Conclusion
In patients with previous CABG undergoing repeat coronary angiography, the femoral vascular access route was associated with greater procedural success but increased access-site bleeding, a result which needs confirmation in other centres, and may justify a randomised trial to provide definitive evidence of benefit or harm in this complex patient group.
Key messages
- The favoured practice of radial access coronary angiography is based on randomised trials that excluded patients with previous coronary artery bypass graft surgery (CABG)
- One in 12 patients undergoing coronary angiography have had previous CABG
- New non-randomised data indicate lower procedural success with radial compared with femoral access angiography in patients with previous CABG and a lower rate of bleeding
- A randomised trial would be useful to determine the preferred approach to investigating this complex subset of patients
Conflicts of interest
None declared.
Funding
None.
Acknowledgement
We are grateful to Miles Curtis for assistance in retrieving study data.
Study approval
The project was registered as an audit with the Clinical Effectiveness Unit of St. Bartholomew’s Hospital NHS Trust and did not require ethical approval.
References
1. Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States: 2001–2008. JAMA 2011;305:1769–76. https://doi.org/10.1001/jama.2011.551
2. British Cardiovascular Intervention Society. BCIS audit returns. Adult interventional procedures. Jan 2016 to Dec 2016. Available from: http://www.bcis.org.uk/wp-content/uploads/2018/03/BCIS-Audit-2016-data-ALL-excluding-TAVI-08-03-2018-for-web.pdf
3. Hamon M, Mehta S, Steg PG et al. Impact of transradial and transfemoral coronary interventions on bleeding and net adverse clinical events in acute coronary syndromes. EuroIntervention 2011;7:91–7. https://doi.org/10.4244/EIJV7I1A16
4. Rao SV, Ou FS, Wang TY et al. Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention; a report from the National Cardiovascular Data Registry. J Am Coll Cardiol Interv 2008;1:379–86. https://doi.org/10.1016/j.jcin.2008.05.007
5. Chodór P, Krupa H, Kurek T et al. RADIal versus femoral approach for percutaneous coronary interventions in patients with Acute Myocardial Infarction (RADIAMI): a prospective, randomized, single-center clinical trial. Cardiol J 2009;16:332–40. Available from: https://journals.viamedica.pl/cardiology_journal/article/view/21480/17084
6. Cooper CJ, El-Shiekh RA, Cohen DJ et al. Effect of transradial access on quality of life and cost of cardiac catheterization: a randomized comparison. Am Heart J 1999;138(3 Pt 1):430–6. https://doi.org/10.1016/S0002-8703(99)70143-2
7. Agostoni P, Biondi-Zoccai GG, de Benedictis ML et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures: systematic overview and meta-analysis of randomized trials. J Am Coll Cardiol 2004;44:349–56. https://doi.org/10.1016/j.jacc.2004.04.034
8. Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J 2009;157:132–40. https://doi.org/10.1016/j.ahj.2008.08.023
9. Jolly SS, Yusuf S, Cairns J et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 2011;377:1409–20. https://doi.org/10.1016/S0140-6736(11)60404-2
10. Romagnoli E, Biondi-Zoccai G, Sciahbasi A et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol 2012;60:2481–9. https://doi.org/10.1016/j.jacc.2012.06.017
11. Brueck M, Bandorski D, Kramer W et al. A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc Interv 2009;2:1047–54. https://doi.org/10.1016/j.jcin.2009.07.016
12. Wald DS, Wald BJ, Radford A, Shipolini A. The sternal wire code: solving the problem of missing coronary artery bypass graft records during cardiac catheterization. Int J Cardiol Heart Vasc 2018;19:37–40. https://doi.org/10.1016/j.ijcha.2018.04.004
13. Joyal D, Bertrand OF, Rinfret S, Shimony A, Eisenberg MJ. Meta-analysis of ten trials on the effectiveness of the radial versus the femoral approach in primary percutaneous coronary intervention. Am J Cardiol 2012;109:813–18. https://doi.org/10.1016/j.amjcard.2011.11.007
14. Brener MI, Bush A, Miller JM, Hasan RK. Influence of radial versus femoral access site on coronary angiography and intervention outcomes: a systematic review and meta-analysis. Catheter Cardiovasc Interv 2017;90:1093–104. https://doi.org/10.1002/ccd.27043
15. Sanmartin M, Cuevas D, Moxica J et al. Transradial cardiac catheterization in patients with coronary bypass grafts: feasibility analysis and comparison with transfemoral approach. Catheter Cardiovasc Interv 2006;67:580–4. https://doi.org/10.1002/ccd.20633
16. He PY, Yang YJ, Qiao SB et al. A comparison of the transradial and transfemoral approaches for the angiography and intervention in patients with a history of coronary artery bypass surgery: in-hospital and 1-year follow-up results. Chin Med J (Engl) 2015;128:762–7. https://doi.org/10.4103/0366-6999.152488
17. Han H, Zhou Y, Ma H et al. Safety and feasibility of transradial approach for coronary bypass graft angiography and intervention. Angiology 2012;63:103–08. https://doi.org/10.1177/0003319711408863
18. Michael TT, Alomar M, Papayannis A et al. A randomized comparison of the transradial and transfemoral approaches for coronary artery bypass graft angiography and intervention: the RADIAL-CABG Trial (RADIAL Versus Femoral Access for Coronary Artery Bypass Graft Angiography and Intervention). JACC Cardiovasc Interv 2013;6:1138–44. https://doi.org/10.1016/j.jcin.2013.08.004
