The aims of treatment in chronic heart failure are to reduce symptoms, improve function and prolong life. Currently there is no patient-centred health-related quality of life measure in chronic heart failure. The aim of this study was to explore health-related quality of life from the perspective of patients with chronic heart failure and to identify themes for inclusion in a patient-generated instrument.
Semi-structured interviewing of patients with an objective diagnosis of chronic heart failure was undertaken. Analysis of the transcripts identified seven themes on health-related quality of life. These were: changes in physical ability, emotional state, self-awareness and self-perception, changes in relationships, symptoms, maintaining social/lifestyle status and cognitive aspects.
Findings from this study will contribute to the development of a patient-led health-related quality of life measure for use in everyday practical care in a chronic heart failure population.
Introduction
Recently the focus of medical care has shifted towards management of chronic diseases, with the aim of optimising quantity and quality of life.1-3 Chronic heart failure (CHF) has been no exception to this, where the goal of treatment is not only to prolong life, but also to relieve symptoms and improve function.
Quality of life is a reflection of a person’s mental and physical well-being in their everyday life.4 Health-related quality of life (HRQoL) measures the effects of an illness or a treatment from the patient’s perspective. HRQoL measures are particularly useful and important supplements to traditional physiological measures of health status because they describe or characterise what the patient has experienced as a result of healthcare.1
The main clinical symptoms in CHF are dyspnoea, tiredness and fatigue, which affect quality of life through their limiting effect on physical functioning,5 but may also give rise to psychological problems, adverse treatment effects and social limitations.3,6 These factors may lead to individuals withdrawing from activities and social contact, and consequently experiencing a loss of social relationships and social support.7 Increasing severity of CHF leads to the individual being aware of their own mortality, which contributes to depression, sleep disturbances and anxiety.6 Personal relationships, eating, sexual activity and the ability to work are all limited while paralleled by an increasing dependence on others.6
In the past, HRQoL instruments have been seen as time-consuming and unresponsive assessment tools, but since the introduction of shorter, easier to understand and administer tools there has been an increase in their use in clinical trials.8-10 Although these tools are reliable, their validity may be suspect if they do not measure components of HRQoL that are important to the patient. Many instruments are not derived from patient populations but from an expert, medical viewpoint, yet there is no guarantee that medical professionals understand patients’ HRQoL. To maximise the relevance of these items in HRQoL measures they should be derived, wherever possible, from a patient population.
We have shown that all currently available HRQoL measures in CHF are expert driven; there is no suitable patient-derived measure to assess HRQoL in CHF.11 This is a weakness and justifies efforts to devise a truly patient-centred measure. We would hope that the eventual development of this tool would enable its use alongside more conventional physiological measures of health status in CHF.
Materials and methods
The aim of this qualitative study was to explore HRQoL from the perspectives of people with CHF. The sample consisted of 11 patients admitted to a district general hospital with an objective medical diagnosis of CHF between October 2003 and February 2004.
The participants were two women and nine men aged between 57 and 72 years (mean 62 years). All were found to have left ventricular dysfunction (of varying severity, as measured by ejection fraction).
Semi-structured interviews were undertaken to ascertain how people with heart failure viewed their HRQoL using a topic guide drawn from the literature, and which had been piloted to evaluate the sequence of the interview, clarity of wording and questions.
Local Research Ethics Committee approval was obtained. Patients meeting the study entry criteria were identified when they were discharged from hospital and given information about the study. Interviews of those consenting to take part were carried out in the patients’ own home by the first author. Each interview was audio tape-recorded and transcribed in full.
The transcripts were analysed using an iterative process in which emergent issues and analytical themes were identified using framework methodology, which is a systematic method of mapping and charting developing themes.12 Reliability of the codes was ascertained by a second researcher independently coding two interviews (19% of the sample), ensuring that the findings were not simply based on the subjective judgements of one individual researcher.13 The level of concordance between the two coders was calculated using Cohen’s Kappa, and was found to be highly satisfactory (interview 1: Kappa = 0.78, agreement of 86 of 107 codes; interview 2: Kappa = 0.81, agreement of 47 of 57 codes).
Results
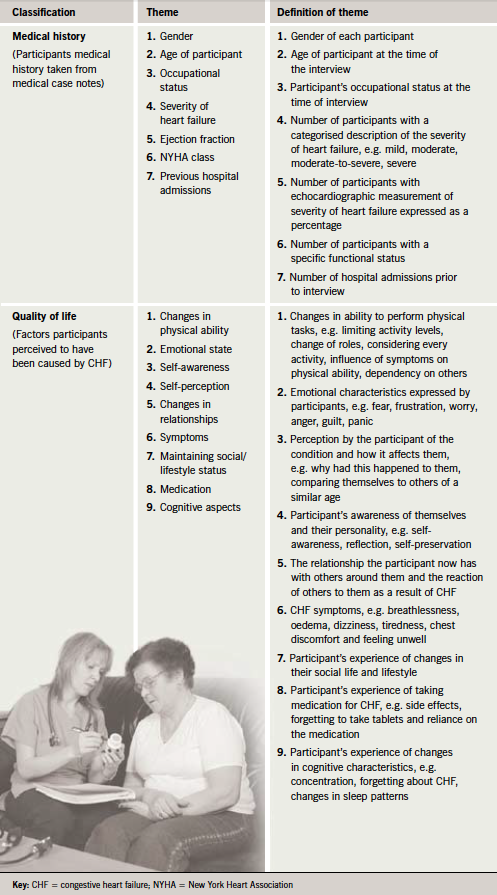
Seven themes on HRQoL were identified. Table 1 shows the definition of classifications and themes. These themes were primarily driven by the data but also reflect theoretically derived dimensions of HRQoL described in other cardiovascular measures.
Changes in physical ability
The most common topic described changes in physical ability, which impacted on all areas of participants’ lives. This theme comprised categories on change of role, considering every activity, limiting activity levels, influence of symptoms and dependency. Participants described how other people in their life were now helping them undertake tasks they would normally have done, which had led to changes in the participants’ roles. Each of these participants saw the changes as negative initially, because they were made to curtail physical tasks before they were ready, or prevented from doing those that they felt they might be able to attempt. Participants expressed a degree of anger and annoyance about this. Most reported that they now thought carefully about undertaking physical exertion due to fear of inducing symptoms, with a resulting limitation in activity levels.
Emotional state
The majority of participants expressed negative emotions, including fear, frustration, worry, anger, guilt and panic. These emotions may arise due to the condition or as a result of the reaction of others towards them because of the condition, or were caused by social issues such as reduced finances. A small number described a feeling of panic that was related to misconceptions of CHF.
Self-awareness and self-perception
This theme includes the perception by the interviewee of the condition and how it affects them. Participants described their perception of the condition in terms of why had it happened to them, discrepancies between the mind and body and comparing themselves to others of a similar age. Participants described aspects that related to self-perception. This included self-awareness, reflection, self-preservation, coping and not being perfect. Coping mechanisms were discussed by participants including: compromise, changing how tasks were undertaken, thinking through activities before doing them, restricting activities, being careful and taking longer to perform tasks. These were employed to reduce the symptoms that any physical activity would create.
Changes in relationships
This theme includes the relationships the participant has with others around them, particularly the spouse and family members, and includes the reaction of others to them as a result of the condition. Participants felt that limitations in life had been imposed on them either by other people or by the condition, including limitations on sexual relationships as a result of fear by their partners that symptoms would manifest during sexual intercourse.
Symptoms
Interviewees described breathlessness, oedema, dizziness, tiredness, chest discomfort and feeling unwell. Breathlessness and tiredness were the most frequently mentioned symptoms and were a problem in relation to physical activity. Every participant mentioned feeling breathless, and most reported that these symptoms were associated with activities of daily living, including activities that involved minimal exertion.
Maintaining social/lifestyle status
Nearly all participants described the impact that CHF had on their lifestyle. This theme included social life, lifestyle, stress, side effects of medication, missing out on life and not giving up. Some participants found that their social life had been reduced, whereas in some it had been enhanced. These changes were often due to tiredness, while some participants described the importance of avoiding stress and how this had affected their HRQoL. Although some participants felt they were missing out on things in life, some participants felt this gave them a new resolve to ensure they didn’t give up.
Cognitive aspects
Most of the participants described cognitive aspects of their life that were affected by the condition. These included changes in concentration, denial or forgetting they had the condition, forgetting to take medication and changes in sleep patterns. In those who described forgetting about the condition, they were reminded by the acute onset of symptoms or by other people reminding them. Several participants described how they had difficulty sleeping or change in their sleep patterns, perhaps caused by the emotional concerns described earlier.
Discussion
This study aimed to explore HRQoL from the perspective of patients with CHF, and to identify themes for inclusion in a patient-generated instrument. The participants described a number of factors that affected their perceptions of how CHF impacted upon them, bringing to light new information regarding HRQoL measures.
Topics not included in current HRQoL measures, but which were identified by this study included: themes of changes in relationships, maintaining social/lifestyle status, forgetting about the condition and medication issues. This finding suggests that HRQoL research among this patient group to date has not been able to fully report their subjective experience, highlighting the importance of producing such measures from the patient perspective. The development of a patient-derived HRQoL measure might help to remedy this deficit.
All participants described the negative effects of having CHF, which reflects the findings in other studies.3,14–16 The limiting of activities may be due to behavioural avoidance as a coping strategy, even though this has been linked to higher mortality in this group of people.17-19 The participants rated the ability to perform tasks and physical activities as the most important aspect of HRQoL, which is echoed in the literature.6,20,21
The participants in this study expressed many negative emotions. Anxiety and fear are commonly reported by people with heart disease, and as early as 1967 Wynn22 reported that unwarranted fear was found in 50% of people post-myocardial infarction. Lee et al.23 found that psychological status was the most prominent factor associated with CHF, suggesting that high levels of anxiety and/or depression would have more severe effects on HRQoL in CHF patients.
A link between extreme health anxiety and physical limitation among people with CHF has been reported,24,25 which suggests that fear and anxiety may promote behavioural avoidance and reduce physical functioning due to a sense of inadequacy in performing activities of daily living.26
The finding that relatives and friends encourage behavioural avoidance is not new. It has been reported in studies of both post-myocardial infarction and angina that relatives may discourage activity because of their fears for the patient.27–29 However, family support had significant effects on participants’ emotional states, which reflects findings from previous research.30,31
In this study all the participants described symptoms that limited them on a daily basis. It is well documented in cancer and chronic obstructive pulmonary disease that breathlessness has a major negative impact on patients’ physical and social functioning and is associated with anxiety.32-34
Some of the participants in this study described cognitive aspects of their life that were affected by CHF. Cognitive dysfunction has been found to be prevalent in this group.35 Reports indicate that patients with CHF display deficits in memory and other intellectual abilities, with unclear clinical relevance.36 Sleep disturbances are very common in patients with CHF.37,38
This study had a number of limitations. There were a small number of participants. The interviews were conducted after the participant had been discharged from hospital and therefore does not address those individuals who have CHF and are diagnosed and treated by their general practitioners.39 The sample contained mostly men with only two women interviewed, although it is accepted that the incidence of heart failure is more common in men than women.40 The average age of the participants was considerably lower than the typical patient with CHF. A truly patient-centred HRQoL measure should take account of the impact of CHF on the HRQoL of family members; this extended impact was not addressed in this study.
To conclude, this study provides a description of how HRQoL is affected by CHF from patients’ perspectives. Themes identified in this study will inform the development of patient-generated items for inclusion in a HRQoL measure. This type of HRQoL measure is sorely needed, as most scales are derived from the viewpoint of health professionals, who may hold different views of which factors are important to HRQoL.41 Psychometric properties of the new measure will be established in subsequent research.
Acknowledgement
The Florence Nightingale Foundation provided general support through The Band Trust Scholarship award.
Conflict of interest
None declared.
Key messages
- Patients’ beliefs about how chronic heart failure affects their health-related quality of life have been identified
- Emotional dimensions of health are more important than the physical dimensions
- The development of a patient-centred health-related quality of life measure is important given the scarcity of such measures in coronary heart disease
References
- Deyo R. The quality of life, research and care. Ann Intern Med 1991;114:695–7.
- Fallowfield L. Quality of life data. Lancet 1996;348:421–2.
- Johansson P, Agnebrink M, Dahlstrom U, Brostrom A. Measurement of health-related
quality of life in chronic heart failure, from a nursing perspective – a review of the literature. Eur J Cardiov Nursing 2004;3:7–20. - Nicolson P, Anderson P. Quality of life, distress and self-esteem: a focus group study of people with chronic bronchitis. Br J Health Psychol 2003;8:251–70.
- Dracup K, Walden JA, Stevenson LW, Bracht ML. Quality of life in patients with advanced heart failure. J Heart Lung Transplant 1992;11(2 part 1):273–9.
- Berry C, McMurray J. A review of quality of life evaluations in patients with congestive heart failure. Pharmacoeconomics 1999;16:247–71.
- Murberg TA, Bru E. Social relationships and mortality in patients with congestive heart failure. J Psychosom Res 2001;51:521–7.
- Hunt SM, McEwen J, McKenna SP. Measuring health status: a new tool for clinicians and epidemiologists. J R Coll Gen Pract 1985;35:185–8.
- The SOLVD investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991;325:293–302.
- MERIT-HF Study Group. Effect of metroprolol CR/XL in chronic heart failure: metroprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet 1999;353:2001–07.
- Dunderdale K, Thompson DR, Miles JNV, Beer SF, Furze G. Quality-of-life measurement in chronic heart failure: do we take account of the patient perspective? Eur J Heart Failure 2005;7:572–82.
- Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess R (eds.). Analysing qualitative data. London: Routledge, 1994;173–94.
- Pope C, Ziebland S, Mays N. Analysing qualitative data. In: Pope C, Mays N (eds.). Qualitative research in health care. London: BMJ Books, 2000;75–88.
- Stull DE, Starling R, Haas G, Young GB. Becoming a patient with heart failure. Heart Lung 1999;28:284–92.
- Juenger J, Schellberg D, Kraemer S et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart 2002;87:235–41.
- Bennett S, Oldridge NB, Eckert GJ et al. Comparison of quality of life measures in heart failure. Nurs Res 2003;52:207–16.
- Denollet J, Brutsaert DL. Personality, disease severity, and the risk of long-term cardiac events in patients with a decreased ejection fraction after myocardial infarction. Circulation 1998;97:167–73.
- Murberg TA, Bru E, Aarsland T. Personality as predictor of mortality: a two-year follow-up study. Pers Individ Dif 2001;31:749–57.
- Murberg TA, Furze G, Bru E. Avoidance coping styles predict mortality among patients with congestive heart failure: a six-year follow-up study. Pers Individ Dif 2004;36:757–66.
- Wenger N, Mattson M, Furberg C, Elinson J. Assessment of quality of life in clinical trials of cardiovascular therapies. Am J Cardiol 1984;54:908–13.
- Fitzpatrick R, Fletcher A, Gore S, Jones D, Spiegelhalter D. Quality of life measures in health care. I: Applications and issues in assessment. BMJ 1992;305:
1074–7. - Wynn A. Unwarranted emotional distress in men with ischaemic heart disease. Med J Aust 1967;18:394–413.
- Lee DT, Yu DS, Woo J, Thompson DR. Health-related quality of life in patients with congestive heart failure. Eur J Heart Failure 2005;7:419–22.
- Murberg T, Bru E, Sveback S, Aarsland T, Dickstein K. The role of objective health indicators and neuroticism in perceived health and psychological well-being among patients with chronic heart failure. Pers Individ Dif 1997;22:867–75.
- Doering L, Dracup K, Caldwell M et al. Is coping style linked to emotional states in heart failure patients? J Card Fail 2004;10:
344–9. - Franks P, Campbell TL, Shields CG. Social relationships and health: the relative roles of family functioning and social support. Soc Sci Med 1992;34:779–88.
- Petrie KJ, Weinman JA. Illness representations and recovery from myocardial infarction. In: Petrie K, Weinman J (eds.). Perceptions of health and illness. Amsterdam: Harwood Academic Publishers, 1997;441–65.
- Furze G, Lewin RJP, Roebuck A, Bull P, Thompson DR. Attributions and misconceptions in angina: an exploratory study. J Health Psychol 2001;6:501–10.
- Roebuck A, Furze G, Thompson DR. Health-related quality of life after myocardial infarction: an interview study. J Adv Nurs 2001;34:787–94.
- Martensson J, Karlsson JE, Fridlund B. Male patients with congestive heart failure and their conception of the life situation. J Adv Nurs 1997;25:579–86.
- Martensson J, Karlsson JE, Fridlund B. Female patients with congestive heart failure: how
they conceive their life situation. J Adv Nurs 1998;28:1216–24. - Skilbeck J, Mott L, Page H, Smith D, Hjelmeland-Ahmedzai S, Clark D. Palliative care in chronic obstructive airways disease: a needs assessment. Palliat Med 1998;12:245–54.
- O’Driscoll M, Corner J, Bailey C. The experience of breathlessness in lung cancer. Eur J Cancer Care 1999;8:37–43.
- Silvester S, Booth S, Todd C. The experience of breathlessness: a qualitative approach. Psychol Health 2000;12:677–89.
- Zuccala G, Onder G, Marzetti E et al. Use of angiotensin converting enzyme inhibitors and variations in cognitive performance among patients with heart failure. Eur Heart J 2005;26:226–33.
- Almeida OP, Flicker L. The mind of a failing heart: a systematic review of the association between congestive heart failure and cognitive functioning. Intern Med J 2001;31:290–5.
- Bradley TD, Floras JS. Pathophysiologic and therapeutic implications of sleep apnea in congestive heart failure. J Card Fail 1996;3:223–40.
- Brostrom A, Stromberg A, Dahlstrom U, Fridlund B. Patients with congestive heart failure and their conceptions of their sleep situation. J Adv Nurs 2001;34:520–9.
- McMurray JJ, Cleland JGF. Heart failure in clinical practice. 2nd ed. London: Martin Dunitz, 2000.
- Petersen S, Rayner M, Wolstenhome J. Coronary heart disease statistics: heart failure supplement. George C, (ed.). Ref Type: Report. London: British Heart Foundation, 2002;9–11.
- Paul S, Sneed N. Patient perceptions of quality of life and treatment in an outpatient congestive heart failure clinic. Congest Heart Fail 2001;8:74–9.
