This year’s Heart Rhythm Congress (HRC 2012), held in Birmingham from 23rd-26th September, was the largest to date showing the growing interest in this specialty. Drs Janet McComb, André Ng, Henry Purcell, and Andreas Wolff report their highlights from the meeting.
Stroke risk assessment in AF
New insights on stroke risk assessment were provided by Dr Ami Banerjee (University of Birmingham), in a session supported by the Atrial Fibrillation Association.
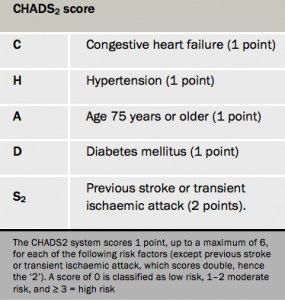
The CHADS2 risk stratification scoring system (table 1) is currently the indicator for the Quality and Outcomes (QoF) framework used to determine whether an atrial fibrillation (AF) patient warrants anticoagulation. It may underestimate risk and those with a score of zero may actually be at substantial stroke risk. He also pointed out that the system has inherent disadvantages. It does not include many of the risk factors for stroke, it has been derived from historical data sets, and it does not identify patients at low risk of stroke.
“Truly low risk, is the new target for risk prediction,” says Dr Banerjee, who thinks the preferred prediction tool should be CHADS2DS2VASc (table 2) – as advocated in the updated (2012) guidelines for the management of AF from the European Society of Cardiology (ESC) – since it takes into account vascular disease, age 65-74 years and gender. Thus patients with a CHADS2DS2VASc score of zero or those under 65 years, and lone AF irrespective of gender, have a truly low stroke risk and do not need anticoagulation.
Bleeding risk, how to assess it and how to stop it

“All anticoagulants increase bleeding,” Dr Joe DeBono (University Hospitals, Birmingham) reminded delegates. With warfarin, an indication of anticoagulation activity is given by the INR (with a target of 2-3 for most indications), and reversing its use – with a prothrombin complex concentrate (PCC) and frozen plasma, for example – is fairly straight forward. In contrast, it is difficult to assess activity with the novel oral anticoagulants (NOACs), which are without “proven antidotes” but they do have shorter half-lives (T1/2), he said. They appear to reduce intracranial haemorrhage (ICH) but they may increase gastrointestinal bleeding.
He asked whether the lack of an antidote mattered. Possible reversal strategies for all anticoagulants include use of activated charcoal, and PCC (very expensive and effective in reversing warfarin but its effects with NOACs are less clear). Most bleeds with NOACs appear to be non-fatal and mild, with the latter responding to local haemostatic measures while more serious bleeds may require fluid replacement and fresh frozen plasma. It is key “to get an early haematological opinion”, said Dr DeBono.
He also considered what should be done if patients need an operation or other intervention, as was the case in a quarter of patients during the RE-LY trial, for example. With NOACs having short half-lives, it may be possible to delay the procedure for a day or two while clotting tests may also be useful. Dialysis or reversal agents should be considered but it is important to avoid neuraxial blockade e.g. epidural anaesthesisa and anticoagulants, he said.
“Prevention is better than cure,” he concluded, reminding delegates not to angticoagulate low-risk patients.
The aspirin conspiracy
This was the intriguing title of a presentation from Dr Matt Fay (Westcliffe Medical Practice, Shipley). He gave a history of the clinical use of aspirin and its associated myths, from its ancient non-aceylated form (around 400 BC) up to modern times. He concluded that aspirin is “clearly inferior to oral anticoagulants” in stroke prevention in AF, especially in the elderly, and it carries a similar bleeding risk to OACs. Dr Fay has been instrumental in promoting the view that in AF patients, at moderate to severe risk of stroke, “we should stop thinking aspirin and start thinking oral anticoagulants”.
Anticoagulation is about three times more effective than aspirin in preventing AF-related stroke but about 53% of AF diagnosed patients are treated with antiplatelets, such as aspirin. And such patients remain at risk.
“As we get older the likelihood of getting warfarin decreases,” Dr Fay pointed out, especially in those over the age of 80 years, a group who have the most to gain with OACs. The risk of bleeding in those at risk of falls is the most commonly cited reason for not providing anticoagulation. Recent studies have shown, however, that elderly patients on OACs at high risk of falls, did not have a significantly increased risk of major bleeding, and that such a risk is not a valid reason to avoid anticoagulation.
Bleeding assessment
Dr Ron Pisters (University Medical Centre, Maastricht, The Netherlands) presented views on how and why we should assess bleeding. First, he said, think about stroke risk and then the risk of bleeding. AF, he said, is a cardiovascular risk factor and “not an arrhythmia per se”. He highlighted how only 50% of patients receive anticoagulation while 70% warrant it.
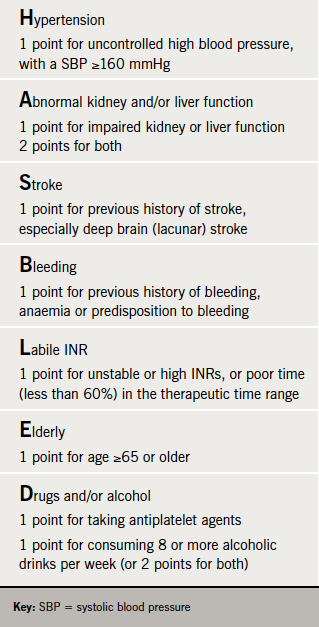
He described how the HAS-BLED score (table 3) has put “bleeding risk on the agenda”. Recommended in the ESC guidelines, HAS-BLED has had “extensive validation” and Dr Pisters believes it should be deployed to “advance the care of AF patients” and reduce the risk of bleeding.
GRASP-AF and cost effectiveness
An important session on stroke prevention in AF was hosted by NHS Improvement. Dr Richard Healicon (National Improvement Lead, NHS Improvement) updated the audience on progress with the GRASP-AF programme, which has seen over 2,200 practices uploading data on 285,000 patients with AF.
The average prevalence of AF has risen to 1.78% suggesting that 900,000 patients in England could suffer from this condition. The latest version of GRASP-AF gives the option of using either the CHADS2 or CHA2DS2VASc risk assessment tool, and CHA2DS2VASc data is available on 26,000 patients so far. Anticoagulation rates have risen very slowly by 2.5%, which means that 44% of patients at high risk of stroke are still not anticoagulated.
Marion Kerr (Insight Health Economics) followed with an insightful economical analysis of stroke prevention in AF based on the latest GRASP-AF data. She estimated that every year 18,000 strokes and 5,500 deaths could be prevented in England with optimal stroke prevention. Potential cost savings to the NHS are around £133 million, while those to society could total £260 million.
Dr Matt Fay spoke about improving stroke prevention and focused on addressing the misconception that aspirin is an effective and safer alternative to anticoagulation in AF. Dr Campbell Cowan (Leeds General Infirmary) highlighted that with the shift to CHA2DS2VASc as the risk assessment tool of choice, the threshold for anticoagulation was lowered significantly at the same time.
Improving management practice of anticoagulation treatment
What makes an optimal anticoagulant? This was the question addressed by Professor Gordon McInnes (University of Glasgow) in a Bayer Healthcare sponsored symposium. All of the anticoagulants we have “are undoubtedly highly effective but have major limitations,” he said. Sometimes they need to be given parenterally and often more than once daily. They all have a potential to cause bleeding and have a narrow therapeutic index. Many have important interactions with other drugs and with foodstuffs. Thus monitoring is often necessary and there is a frequent need for dose adjustment. Onset and offset of drug action is relatively slow, which is a problem if there is a need for rapid effect and, conversely, if you need to stop them because of complications.
Professor McInnes reviewed all the anticoagulant classes and looked at the unmet needs in oral anticoagulants. We need drugs that are:
- rapidly active and can be rapidly inactivated
- have a wider therapeutic margin
- have low potential for food and drug interactions
- require infrequent dose adjustment
- avoid need for monitoring.
This is the challenge, he said, faced by the new oral anticoagulant agents, which inhibit either thrombin or factor Xa (table 4).
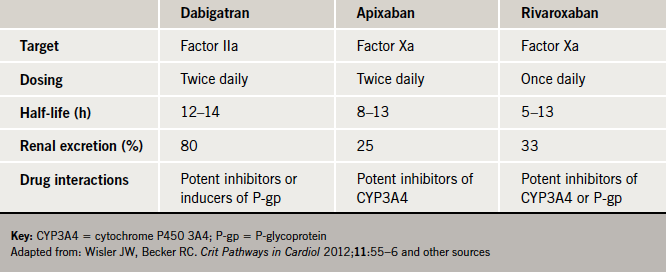
Reviewing the NOACs, which included dabigatran, rivaroxaban and apixaban, he said these offered “real potential” (table 4). All are oral agents and have a relatively brief time to maximum serum concentration and none require anticoagulation monitoring, he said. All have a fairly intermediate half-life – some may be taken once rather than twice daily, which may be an important “practical, pragmatic difference between these drugs,” he said. They also have differences in bioavailability and protein binding.
In terms of drug interactions, Professor McInnes said that there was no evidence so far of interactions with foodstuffs with the NOACs but there is potential for interactions with some powerful enzyme inducers, which tend to be limited to select patient groups, such as those being treated for systemic fungal infections/HIV for example. Focusing on drug clearance, he said that agents such as rivaroxaban and apixaban which favour hepatic metabolism, may offer “a potential safety margin” in patients with renal impairment.
NOACS in treatment and prevention of VTE
Dr Alexander Cohen (Kings College Hospital, London) presented on an unlikely but clinically extremely important topic for HRC – treatment of venous thromboembolism (VTE). He reminded delegates that every year more patients die from VTE than from HIV, breast cancer and road traffic accidents, put together and might account for as many as 60,000 deaths per annum in the UK. In addition VTE can also lead to significant morbidity in the form of pulmonary hypertension and post-thrombotic syndrome. He presented “secondary prevention” data comparing NOACs with standard therapy of parenteral anticoagulant plus warfarin, with emphasis on the EINSTEIN programme utilising rivaroxaban,. EINSTEIN-DVT and EINSTEIN-PE both demonstrated non- inferiority over standard therapy in terms of preventing recurrent thromboembolism with comparable safety data to the warfarin-based regime. A similar finding was seen with dabigatran in the RE-COVER programme.
EINSTEIN-Extension compared the safety and efficacy of rivaroxaban to placebo in the secondary prevention of recurrent symptomatic venous thromboembolism, by prolonging preventative treatment by six or 12 months beyond a completed course of anticoagulation therapy. This showed that in the placebo group the recurrence rate was significant at 7.1% and that rivaroxaban reduced recurrence by 82%, at the cost of a slight increase in bleeding complications.
Devices, leads and other complications
One of the highlights of the conference was a session devoted to a lead used with implantable cardioverter defibrillators, which is prone to early failure (St Jude Medical Riata), and which is the subject of medical device alert issued by the Medical Healthcare products Regulatory Agency (MHRA). Delegates learned about the construction of defibrillator leads and how the next generation lead is less likely to fail. This session also covered the management of such patients, looking at the risks of leaving in leads at risk of failure against the risks of replacing them, highlighting the precautions that can be taken to detect failure as soon as it occurs. Clear clinical pointers were given on how to improve practice.
Another very interesting session examined complications of device implantation. It is becoming clear that complications of pacemaker and defibrillator implantation are more common than realised. A call was given for the need to collect robust data and also to reduce complications by ensuring devices are only implanted by competent operators in competent centres.
Management of syncope
In a session on syncope, impressive data were presented from the Manchester Heart Centre rapid access blackout clinic on the diagnosis of the cause of syncope. In a discussion on drugs used to try and prevent syncope, the need to review medication was emphasised – some drug therapy, particularly in the older patient with postural hypotension, should be withdrawn.
Highlights from abstracts, posters and basic sciences
The scientific sessions saw vibrant contribution from many electrophysiology and device centres showcasing data from the latest in cutting-edge research to good clinical practice. Around half of 130 abstracts submitted were selected for presentation as oral and poster (moderated and standard) communications.
Presentations included risk stratification for sudden cardiac death, which continues to be an important research area including promising data from a new proposed algorithm, data on the use of scar and fibrosis from cardiac magnetic resonance imaging (MRI) and other markers in predicting mortality. Data on new technologies and practices in AF ablation were presented, which included contact force catheters, use of MRI to evaluate post-ablation lesions and data on a more widespread practice of uninterrupted warfarin for ablation.
Several presentations looked at the subject of Patient Reported Outcome Measures (PROMs) in ablation procedures with data collected from three electrophysiology centres. The implications of the reporting of these measures in the context of commissioning for procedures were highlighted in addition to the value of using generic tools, which provide measures that can be compared with other surgical operations.
The high incidence of AF in pacing populations (identified with pacemaker interrogation) was presented, especially the importance that when asymptomatic, patients may not receive appropriate antithrombotic therapy. Data were presented from two separate centres on the practice of pacemaker implantation following open heart surgery. AF incidence appeared to be related to surgical complexity.
There was continued important contributions from basic science preclinical mechanistic studies at the congress. A new feature this year was a separate Allied Professionals oral presentation session, which received very positive feedback. Delegates heard of an interesting change in clinical risk score data on implantable cardioverter defibrillator (ICD) patients between implant and generator replacement, experience of an extended catheter lab nurse role in implanting loop recorders and paramedic treatment of supraventricular tachycardias.
Awards
The Young Investigators Award competition continues to be a main feature of the Congress. Top quality research work from the six shortlisted presenters included the importance of autonomic cardiac control during AF ablation and in Brugada syndrome, interesting data on coronary flow with cardiac resynchronisation therapy, basic science data in MRI lesions following acute ablation, and on the dynamic behaviour of electrical signals during persistent AF.
Congratulations to Louisa Malcolme-Lawes (Imperial College London) who won the Young Investigators Clinical Award and to James Harrison (King’s College London) who won the Young Investigators Basic Science Award.
The Arrhythmia Alliance Excellence in Practice Awards were also presented during the congress. Congratulations to Martin Harman who won The Charles Lobban Volunteer Award for Outstanding Contribution to Arrhythmia Services – after being diagnosed with AF at the age of 29, he has raised awareness on both national and international levels through fundraising marathons and local publicity. Dr Carolyn Dean received the Award for Outstanding Medical Contribution to Cardiac Rhythm Management for her research into how magnesium deficiency affects arrhythmia conditions. Ms Melloney Ferrar (Sheffield Teaching Hospitals NHS Foundation Trust) won The Allied Professional Award for Outstanding Contribution to Arrhythmia Management for her work in establishing one of the first clinics solely for postural orthostatic tachycardia syndrome patients. Professor Gregory Lip and Dr Deirdre Lane (University of Birmingham, Centre for Cardiovascular Sciences) won the Team of the Year Award for their collaboration to improve bleeding risk assessment for AF patients.
HRC 2012 highlights
- The channelopathies session, which focused on current understanding in genetics and what to do when syndromes such as long QT and Brugada are found
- A first class device follow-up master class, with presentations from highly experienced physiologists including Sue Jones (St George’s London) who shared their experience and expertise
- The popular “Cases and traces” session where challenging cases were presented by electrophysiologists from around the UK
- The new exhibition hall, which housed 50 exhibitors from industry, charities and other organisations, and held events, such as the launch of The Heart of AF website (www.heartofaf.org). This new websiste, produced by the AF Association, has been designed as a one-stop destination for researchers, clinicians and aligned professionals with an interest in AF and the improvement of its management
- The abstract posters – showcased in the exhibition hall – with 68 accepted into the scientific programme. All accepted abstracts were published in Europace 2012;14 (suppl 4).
HRC 2013 will take place on 20th-23rd October 2013 at the ICCC, Birmingham
Contributors
Dr Janet Mc Comb, Consultant Cardiologist
Freeman Hospital, Newcastle
Dr G André Ng, Consultant Cardiologist and Electrophysiologist
University of Leicester / University Hospitals of Leicester, Glenfield Hospital
Dr Henry Purcell, Senior Fellow in Cardiology
Royal Brompton Hospital, London
Dr Andreas Wolff, General Practitioner
Whinfield Medical Practice, Darlington
Please note the pdf for this report is an abbreviated version of the above report. The HRC report follows on from the ESC coverage in this pdf.
