Introduction
Infective endocarditis (IE) is uncommon but important because it is difficult to manage and universally fatal unless appropriately treated. The estimated incidence is 3–10 episodes per 100,000 population each year,1 and this is gradually rising although the reasons for the increase are not known.2,3 Most cardiothoracic centres see between 50–100 cases per year.2
The epidemiology of IE is changing.4 In industrially developed countries, increasing numbers result from infection of pacing devices, replacement heart valves and medical interventions such as haemodialysis.
The average age of patients with IE is increasing4 but younger age-groups are also affected, particularly intravenous drug users (IVDU) and those with adult congenital heart disease.5 Predisposing factors include diabetes, cancer and haemodialysis.6
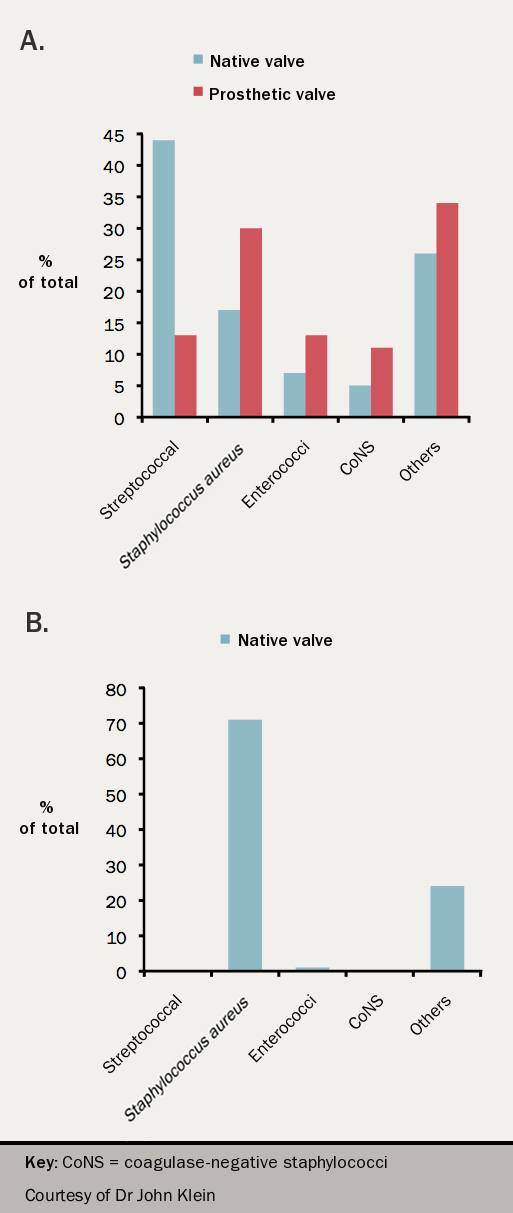
The most common organisms causing native valve IE in non IVDU are the oral streptococci followed by staphylococci and enterococci (see figure 1) while in IVDU the predominant organism is Staphylococcus aureus. After device implantation, prosthetic valve or pacemaker, staphylococci predominate (both S aureus and coagulase negative staphylococci (CNS)). Late prosthetic valve endocarditis (occurring one year after surgery) is most often caused by oral streptococci.
In-hospital mortality is high, about 20%7 and is associated with:
- delayed diagnosis,
- prosthetic valve involvement,
- increasing age,
- heart failure
- staphylococcal infection.6,7
When to suspect IE
It should be suspected if there is:
- Fever with underlying structural heart disease or intracardiac device
- Fever and new murmur of valve regurgitation
- Fever with vasculitic lesions or stroke
- A suspicious organism in blood cultures (e.g. S. aureus or community acquired Enterococcus faecalis) or persistently positive blood cultures
- A splenic infarct(s)/abscess or haematogenous spinal infection or brain abscess
- Staphylococcus aureus bacteraemia related to a line but only if the fever fails to settle within 48 hours or blood cultures remain positive after 72 hours or there are emboli or other features suggestive of IE
