A patient with inappropriate tachycardia is described who failed to respond to beta blockers or calcium channel blockade but had clinical improvement with ivabradine. The heart rate slowing with this drug was illustrated by the change in the R–R interval histogram.
Case report
A 62-year-old woman was referred to the cardiology clinic for investigation of troublesome palpitations associated with a persistent fast heart rate. Her symptoms had been present for at least 10 years. She was usually fit and well and had a normal exercise tolerance. She was an ex-smoker of 20 pack-years and had a moderate intake of alcohol and caffeine. Her previous medical history, family history and clinical examination were unremarkable. Her resting electrocardiogram (ECG) was normal except for sinus tachycardia. The P waves were prominent and showed normal axis and morphology. Causes of secondary sinus tachycardias were excluded with normal routine blood tests including thyroid function tests and normal urinary catecholamines.
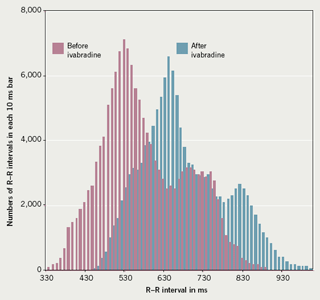
A 24-hour ambulatory ECG record demonstrated sinus tachycardia throughout with a mean heart rate of 106 beats per minute. Analysis of the R–R interval histogram before she received any medication showed two broad peaks: the larger corresponded to a peak rate of 117 beats per minute and the smaller to a peak rate of 88 beats per minute (figure 1).
More than one peak with an R–R interval histogram is not abnormal. Minor differences in P-wave morphology were seen that appeared to correlate with these peaks and these are presumed to reflect normal physiological shifts in the origin of the sinus node site of depolarisation. There was no orthostatic response with standing or tilting to suggest postural orthostatic tachycardia syndrome. With an exercise treadmill test, the heart rate increased progressively from 117 beats per minute at rest, reaching a maximum at 7 metabolic equivalents tasks (METs) peak exercise of 176. This was higher than the predicted normal of 155 beats a minute.
The initial management of her tachycardia was with a beta blocker, which was poorly tolerated. A long-acting preparation of diltiazem only achieved a small reduction of her heart rate with no symptomatic improvement. She was then prescribed ivabradine increasing to 7.5 mg twice daily. This was an off-label use of this medication but we hypothesised that given its mechanism of action it was likely to be effective in controlling this patient’s tachycardia. On review one month later, her symptoms had improved considerably and her resting heart rate was slower. A further 24-hour ambulatory ECG and R–R interval histogram confirmed the reduction of mean heart rate from 106 beats per minute prior to ivabradine, compared with 89 beats per minute while receiving this drug. The two preferential heart rate peaks remained as previously (figure 1). At follow-up 18 months later she remained well on the same medication.
Discussion
Sinus tachycardias are a heterogeneous group of disorders and have received more attention in recent years in the literature as understanding of the pathophysiology of the sinus node improves.1 In our patient, there was no evidence of a secondary response to other illness or stimulant drugs and the appearances of the ECG and histogram did not suggest a discrete electrical atrial tachycardia. Such patients are labelled as having an ‘inappropriate sinus tachycardia’. The response to conventional medication is often disappointing and invasive approaches have included catheter modification or even excision of the node. Recently, a selective Ifinhibitor, ivabradine, acting selectively on the sinus node, has been shown to significantly reduce heart rate and has been successful in improving symptoms in stable angina. It has also been suggested that the use of ivabradine for inappropriate sinus tachycardia may be a ‘marriage made in heaven’.2
Ivabradine proved very successful in managing inappropriate sinus tachycardia in this patient. The R–R interval histogram is a simple means of demonstrating heart rate variability,3 and we believe that this is the first time that the effects of this medication have been demonstrated in this way.
Conflict of interest
None declared.
References
- Yusuf S, Camm AJ. Deciphering the sinus tachycardias. Clin Cardiol 2005;28:267–76.
- Yusuf S, Camm AJ. Sinus tachyarrhythmias and the specific bradycardic agents: a marriage made in heaven? J Cardiovasc Pharmacol Ther 2003;8:89–105.
- Crook BR, Cashman PM. The R–R interval histogram. Postgrad Med J 1976:52(Suppl 7):46–53.
