The National Institute for Health and Clinical Excellence (NICE) has issued guidance on the investigation of patients with recent onset of chest pain, recommending CT calcium scoring (CAC) as the preferred test in some low-risk groups. This reflects concern about the low sensitivity (high false positive rate) of exercise stress tests (EST). This represents a major shift away from traditional rapid-access EST clinics and has generated concern. We looked at 125 consecutive ungraded patients with equivocal ESTs referred for CAC, and CT coronary angiography (CTA), if required. We found that 53% of patients had a CAC = 0 and would need no further testing under the NICE protocol. We estimate this would rise up to 70–80% if only low likelihood patients were studied. Two per cent of patients with a CAC = 0 required coronary intervention.
As per NICE protocol, all patients with a CAC between 1 and 400 underwent CTA, and, of these, 25% required invasive coronary angiography (ICA) and 17% underwent coronary intervention.
The overall strategy of CAC followed by CTA (if CAC between 1 and 400) and ICA (if CAC >400) produced a final sensitivity of 88% (higher than EST) and a negative predictive value of 98% (similar to EST). We believe the strategy is a useful way to assess recent onset chest pain but concerns about radiation dose, availability and patients with obstructive non-calcific plaque remain.
Introduction
In March 2010, the National Institute for Health and Clinical Excellence (NICE) issued guidance on the assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin.1 The paper emphasised calculating the likelihood of coronary artery disease (CAD), before considering diagnostic investigations, based on 12-lead electrocardiogram (ECG) findings and initial clinical assessment.
Briefly, the guidance suggests people with a high pre-test likelihood that chest pain is due to angina (61–90%) but with an uncertain diagnosis should go straight to invasive coronary angiography (ICA), while those with a moderate pre-test likelihood (30–60%) should be considered for non-invasive functional imaging tests, such as nuclear myocardial perfusion scan (MPS), stress echocardiography (SE) and cardiac magnetic resonance imaging (MRI). Those with a low pre-test likelihood (10–29%) were recommended for coronary artery calcium (CAC) scoring. Estimation of risk is based on age, gender and presence of three risk factors, as well as a clinical assessment score based on the characteristics of the chest pain.
This represents a major departure from the traditional exercise stress test (EST) performed in a rapid access chest pain clinic (RACPC) and has attracted some criticism in the medical press, focusing on the risks to a vulnerable population of delayed access to tests.2,3 NICE, in turn, believes that EST poses particular problems of poor sensitivity (high false positive rate) or difficulties in interpretation in women, diabetics and patients with conduction defects, such as left bundle branch block, among others.4 A meta-analysis of over 24,000 patients undergoing both EST and ICA yielded an overall sensitivity of 71% with specificity of 73% for EST.5 Ideally, a test to exclude the presence of a condition should have a high sensitivity (the test recognises all actual positives) and high negative predictive value (the test generates few false negatives). EST has an excellent negative predictive value of around 97%.6
Our centre has performed both EST and 64 multi-detector cardiac computed tomography (64-MDCT) since 2007. Although 74% of patients leave our RACPC with a negative result, the remaining 26% require additional tests including ICA, 64-MDCT, SE and MPS. We have previously documented higher false positive EST rates (p<0.001) and more equivocal results (p<0.01) among women.7
Methods
To assess the implications of CAC screening for low-risk chest pain patients, we analysed results and outcomes from 125 consecutive patients without previous heart disease who underwent EST for chest pain or discomfort and, in view of equivocal EST result, were then referred for CAC followed by coronary CT angiography (CTA) if appropriate. Patients were not graded for pre-test likelihood on EST.
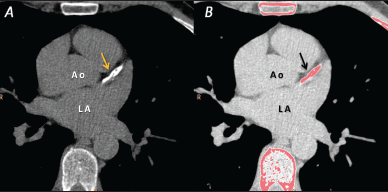
CAC (radiation dose 1–2 mSv) was calculated using the Agatston scoring method8 (figure 1) and, if the heart rate was less than 64 bpm and stable, a low dose, prospectively ECG triggered (pECG) CTA study was performed, otherwise a retrospectively ECG gated (rECG) protocol was used.9 In the NICE guidance, CAC was graded into three categories:
- CAC = 0; other chest pain causes should be investigated.
- CAC = 1–400; CTA should be offered.
- CAC >400; ICA should be offered.
In our analysis, all patients with a CAC = 0 underwent CTA because of prior equivocal EST findings, affording an opportunity to assess false negatives with a CAC = 0, as well as the sensitivity and negative predictive value of the overall strategy outlined above.
Results
The results, including catheterisation and intervention rates are shown in table 1. A two-tailed Fisher’s exact test was used to compare each group with CAC = 0. A low-dose pECG protocol was used in 55% of patients undergoing CTA.

1. CAC = 0
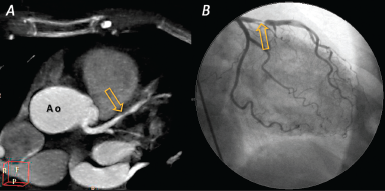
Sixty-six patients (53%) were in this category (74% female, mean age 51 years). All had CTA. Three (5%) underwent ICA as CTA suggested significant non-calcific plaque. One had non-obstructive plaque (55-year-old female, high pre-test likelihood), one had an occluded right coronary artery (58-year-old male, high pre-test likelihood), and one (2%) needed percutaneous coronary intervention (PCI) (65-year-old female, low pre-test likelihood) (figure 2).
2. CAC between 1 and 400
Forty-eight patients (38%) were in this category (44% female, mean age 59 years). Median CAC was 52. All had CTA with ICA recommended in 12. Eight required PCI. The remainder had non-obstructive plaque. The catheterisation (25%) and intervention rates (17%) were significantly higher (p<0.01) than for patients with CAC = 0.
3. CAC >400
Eleven patients (9%) had a CAC >400 (27% female, mean age 63 years). CAC ranged from 440 to 2,825 with a median of 782. CTA was performed in two (CAC <452) with no obstructive plaque seen. The remainder (CAC >577) had ICA. Of these nine patients, three required coronary artery bypass grafting (CABG) and four PCI. The catheterisation (82%) and intervention rates (64%) were significantly higher (p<0.001) than for patients with CAC = 0.
4. Any CAC >0
Adding groups 2 and 3 together yields patients with a CAC >0. Fifty-nine patients (47%) were in this category (41% female, mean age 60 years). Median CAC was 78. ICA was recommended in 21. Fifteen required PCI or CABG. The catheterisation (36%) and intervention rates (25%) were significantly higher (p<0.001) than for patients with CAC = 0.
Overall, the NICE strategy of CAC followed with CTA or ICA based on a positive CAC score yielded a final sensitivity of 88%, a specificity of 94%, a positive predictive value of 71% and a negative predictive value of 98%.
Discussion
Reliability of CAC as a test of exclusion
The diagnostic and prognostic value of calcium scoring was recently systematically reviewed in over 85,000 symptomatic and asymptomatic patients.10 Seven studies in the review assessed prognosis in symptomatic adults (3,924 patients), over a follow-up period of 30 to 84 months, a CAC = 0 was associated with a cardiovascular event rate of 1.8% versus an event rate of 8.99% with CAC >0 (p<0.0001). Eighteen studies examined 10,355 symptomatic patients undergoing both CAC and ICA. Only 131 out of 5,805 patients with significant CAD had a CAC = 0 (2%). Thus, a CAC = 0 comes close to effectively ruling out obstructive CAD. Patients with a positive CAC should be advised about a healthy lifestyle and
coronary risk assessed if CTA reveals no obstructive plaque.11
Patients with obstructive plaque and no coronary calcium are more likely to be young and present with unstable symptoms.12 Diabetics are also more likely to present with non-calcified plaque.13
The sensitivity and negative predictive values in our small analysis compare well with a study of 1,851 symptomatic patients undergoing both CAC and ICA.14 In that study, sensitivity was 95% and specificity was 66% with a negative predictive value of 98%.
Impact on workload
At present, approximately 5% of all patients attending our RACPC undergo CAC and CTA.7 We also know that 28% of referrals to our RACPC have a low pre-test likelihood of CAD.7 Based on these figures, we could expect a five- to sixfold increase in the number of patients referred for CT imaging from this source.
In the current analysis (with no selection for pre-test likelihood), we found that 53% of patients had a CAC = 0 and so would not require CTA under NICE guidance. Similarly, 9% had a CAC >400 and would not require CTA (62% in both categories). If only low-risk patients were referred, we would expect more people with CAC = 0 and fewer with CAC >400. It would seem reasonable to estimate that approximately 70–80% would only need CAC; the remaining 20–30% may require both CAC and CTA.
Our area is regarded as having a high prevalence of CAD with 731 patients attending our RACPC in the last year. We can, therefore, estimate that 205 patients would be referred for CAC instead of EST with 40–61 CTAs required. Dividing by our catchment population of 180,000, yields a referral rate of 114 CAC examinations per 100,000 population per year with 22–40 CTAs.
The additional CAC and CTA examinations will, of necessity, compete for scanner and reporting time with other CT examinations, and will require additional appropriately trained staff to perform and report all the studies generated. The NICE guidelines will probably increase demand for functional imaging tests as well.
Estimated radiation burden
The accepted international figure for a year’s background radiation is 2.4 mSv. Coronary CT angiography represents a significant radiation burden with CAC (1–2 mSv) delivering approximately six months’ exposure; pECG CTA (2–4 mSv) one to two years and rECG CTA (7–14 mSv) up to six years’ exposure. By comparison, the accepted average dosage for ICA is 4–7 mSv and MPS (technetium 99m sestamibi, rest and stress protocol) is in the order of 10 mSv. Females and the young are more sensitive to ionising radiation.15 Using the figures obtained in our analysis; 62% of patients (CAC = 0 or >400) would experience 1–2 mSv exposure. As stated above, this would probably rise to 70–80% in low-likelihood patients with the remainder receiving either 2–4 mSv or 7–14 mSv in equal proportion. There is no safe lower limit of X-ray exposure, so the ALARA (as low as reasonably achievable) principle must always be adopted.16 The likelihood of CAD in a young female may be so low as to make a radiation-based test unacceptable. The NICE clinical scoring system yields less than 10% pre-test likelihood in several younger or female groups with more atypical pain, in which case, no investigation is recommended.
Limitations of the analysis
Patients were not graded by pre-test likelihood. Overall, we feel this is acceptable as only a small number of low-likelihood patients would have been available. Our study differs from the NICE protocol in that patients with CAC = 0 underwent CTA, this allowed us to identify false negative CAC results in 2%. Given that patients are already on the CT table and monitored, i.e. ready to go for CTA, it may prove helpful to proceed to CTA if a low radiation dose protocol can be administered to suitable patients. Future developments in CT technology may facilitate this.
Conclusions
We examined the implications of adopting NICE guidance for low-likelihood patients by analysing consecutive, ungraded patients referred for CAC and CTA following an equivocal EST result. We found the overall NICE strategy has a sensitivity of 88% and a negative predictive value of 98% for excluding obstructive coronary disease. Almost three-quarters of patients with a CAC = 0 were female and, on average, were younger than those with a positive CAC. Approximately 2% of patients with a CAC = 0 required coronary intervention. This figure is similar to published studies with diabetes, young age and unstable symptoms identified in the literature as warning signs.
A CAC between 1 and 400 was associated with an ICA rate of 25% and an intervention rate of 17%. We estimate that adoption of the guidance would result in 114 CAC examinations per 100,000 population per year, plus an additional 22–40 CTAs.
Radiation remains a concern, especially in young females, but the sensitivity of CAC is higher than EST with an equivalent negative predictive value. We believe CT calcium scoring will prove a useful and effective test if there is sufficient capacity to perform tests in a timely fashion. We hope our data can inform debate on this controversial topic.
Conflict of interest
None declared.
Key messages
- National Institute for Health and Clinical Excellence (NICE) guidance recommends computed tomography (CT) calcium scoring to assess
some low-risk chest pain patients. High-risk patients go straight to
cardiac catheterisation and
medium-risk patients undergo
stress imaging - Treadmill exercise stress tests (EST) have poor sensitivity in some patient groups. False positives are seen in females with interpretation problems
in diabetics and those with bundle branch block - CT calcium scoring has a higher sensitivity than EST. A calcium score of zero is associated with a low risk of future cardiovascular events. A positive calcium score confirms atherosclerosis with lifestyle modification and cardiac risk assessment required. The radiation dose is equivalent to six months’ background exposure
- Two per cent of patients with zero CT calcium score require coronary intervention. Patients with unstable symptoms, diabetics or young people may develop plaque without calcification
References
- National Institute for Health and Clinical Excellence. Chest pain of recent onset. Assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin. London: NICE, 2010. Available from: http://www.nice.org.uk/guidance/CG95
- Praities N. NICE rules out treadmill test for angina. Pulse 2009;Jun 8. Available from: http://www.pulsetoday.co.uk/story.asp?storycode=4122923
- Praities N. NICE chest pain guidance “could cause dangerous delays”. Pulse 2009;Jun 26. Available from: http://www.pulsetoday.co.uk/story.asp?storycode=4123117
- National Institute for Health and Clinical Excellence. Myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction. Technology Appraisal 73. London: NICE, 2003. Available from: http://guidance.nice.org.uk/TA73/Guidance/pdf/English
- Gianrossi R, Detrano R, Mulvihill D et al. Exercise-induced ST depression in the diagnosis of coronary artery disease. A meta-analysis. Circulation 1989;80:87–98.
- Gibbons RJ, Balady GJ, Bricker JT et al. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee to update the 1997 exercise testing guidelines). Circulation 2002;106:1883–92.
- Purvis JA, Magee H, Sweeney C, Courtney C, Kennedy H, O’Kane J. Additional tests and final outcomes of rapid access chest pain clinic patients with positive or equivocal EST results. Irish J Med Sci 2009;178(suppl 9):S371.
- Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827–32.
- Earls JP. Questions in cardiovascular CT: how to use a prospective gated technique for cardiac CT. J Cardiovasc Comput Tomogr 2009;3:45–51.
- Sarwar A, Shaw LJ, Shapiro MD et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging 2009;2:675–88.
- Erbel R, Mohlenkamp S, Kerkhoff G, Budde T, Schmermund A. Non-invasive screening for coronary artery disease: calcium scoring. Heart 2007;93:1620–9.
- Schuijf JD, van der Wall EE, Bax JJ. Lesions without calcium: lessons from CT angiography. Heart 2009;95:1038–40.
- Sholte AJ, Schuijf JD, Kharagjitsingh AV et al. Prevalence of coronary artery disease and plaque morphology assessed by multi-slice computed tomography coronary angiography and calcium scoring in asymptomatic patients with type 2 diabetes. Heart 2008;94:290–5.
- Budoff MJ, Diamond GA, Raggi P, Arad Y, Guerci AD, Callister TQ. Continuous probabilistic prediction of coronary artery disease using electron beam tomography. Circulation 2002;105:1791–6.
- Einstein AJ. Radiation risk from coronary artery disease imaging: how do different diagnostic tests compare? Heart 2008;94:1519–21.
- Committee to assess health risks from exposure to low levels of ionizing radiation. Board on radiation effects research, division on earth and life studies. National research council. Health risks from exposure to low levels of ionizing radiation: BEIR VII phase 2. Washington DC: The National Academies Press, 2006.
