Atherothrombosis is a leading cause of global mortality. It represents a significant public health issue in the UK and, as such, the UK Government has made it a healthcare priority. The global REduction of Atherothrombosis for Continued Health (REACH) Registry aims to evaluate the long-term risk of atherothrombotic events in an at-risk population, to assess the importance of cross-risk and to define predictors of atherothrombotic events. REACH has recruited over 68,000 people in over 5,000 centres in 44 countries, of which 618 were from the UK.
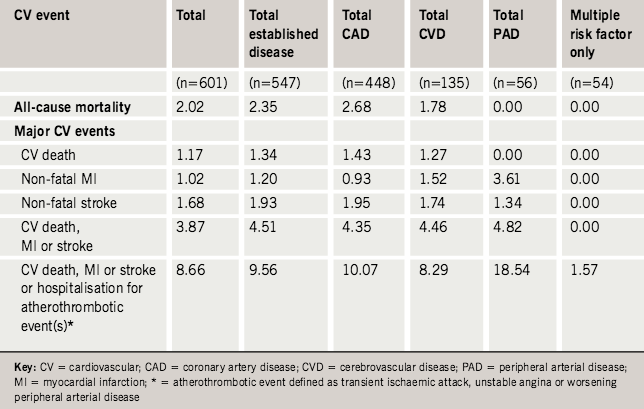
As with the global results, there was a high use of evidence-based therapies in the UK patients. Despite this, the combined incidence of cardiovascular events at one year (cardiovascular death, myocardial infarction, stroke) was high at 4.82%, 4.46% and 4.35% respectively for peripheral arterial disease (PAD), cerebrovascular disease (CVD) and coronary artery disease (CAD). These figures increase markedly when hospitalisations are taken into account, particularly in patients with PAD (18.54%) compared with CVD (8.29%) and CAD (10.07%). Cardiovascular event rates increased significantly with the number of symptomatic locations (p=0.0043), increasing from 8.23% in one location to 16.05% in two, and as high as 18.30% with three symptomatic locations.
The results of the UK cohort are broadly similar to those of the Western European population, and the global registry. It should be a cause of concern that, even with our current cardiovascular risk management, morbidity and mortality remain so high. We need to be doing more to improve cardiovascular outcomes for patients with atherothrombotic disease, particularly those with multi-vascular disease and the much under-recognised PAD.
Introduction
Atherothrombosis is a leading global cause of morbidity and mortality1,2 and its prevalence is growing. Indeed, the Health Survey for England 2004 reported that the total prevalence of ischaemic heart disease and stroke in men had risen from 7.1% of men in 1994 to 9.1% in 2003.3 The increase for women was less, increasing from 5.2% to 6.3% in the same time period.3
The global REduction of Atherothrombosis for Continued Health (REACH) Registry,4-6 aims to evaluate the long-term risk of atherothrombotic events in a global at-risk population, to assess the importance of cross-risk and to define predictors of atherothrombotic events. Results clearly show the high level of cardiovascular morbidity and mortality associated with atherothrombotic disease, even within one year. In particular, they highlight how the multi-vascular disease affecting one in six patients in the registry confers an increased risk for vascular events, not just in the presenting arterial location, but also in others.6 The one-year risk of vascular events defined as cardiovascular (CV) death, myocardial infarction (MI), stroke or hospitalisation for an atherothrombotic event, increased significantly with the number of symptomatic vascular locations, ranging from 5.31% for risk factors only to 12.58% with one, 21.14% with two and 26.27% with three locations (p<0.001 for trend).6 Coexistence of peripheral artery disease (PAD) with either cerebrovascular disease (CVD) or coronary artery disease (CAD) doubles the associated event rates of CV death, MI, stroke, and MI hospitalisation.
This paper presents the one-year analysis of the UK REACH population and provides a comparison to the published data from the global REACH Registry.
Methods
The design and methodology for the REACH registry has been published previously.4 Briefly, REACH is a prospective observational registry of patients at high risk of atherothrombotic events. Over 68,000 patients were enrolled sequentially in more than 5,000 centres in 44 countries, and their outcomes will be followed over four years. This paper covers the results after one year of follow-up of the UK cohort and the data were analysed according to same methodology as for the global registry.4
Results
The UK REACH investigators enrolled 618 patients, 601 of whom were available for follow-up at one year. Demographics of these patients at one year do not differ markedly from those previously reported at baseline.7 The mean (±SD) age of patients was 68.6 (±8.6) years, 62.4% were male, most had symptomatic vascular disease and very few (8.99%) fell into the risk factor only group. Hypertension, hypercholesterolaemia, obesity and diabetes were common at 68.39%, 81.2%, 30.35% and 24.29%, respectively, and many patients were current (15.24%) or former smokers (48.58%). Baseline use of evidence-based medications at one-year follow-up remained high, with 85.76% of patients on antiplatelet agents, 84.53% of patients on lipid-lowering agents and 88.02% of patients on at least one cardiovascular agent.
Overall all-cause mortality at one year was 2.02% with a rate of 2.35% in the symptomatic population: 2.68% for CAD and 1.78% for CVD. Small numbers meant that there were no events in the small PAD or multiple risk factor-only groups (table 1). The overall combined CV death, MI or stroke rate at one year was similar across the symptomatic groups (4.51% overall), but there were no events in the multiple-risk-factor-only group. The rate of the combined end point of cardiovascular events plus hospitalisation was higher in the symptomatic population (9.56%) than in the risk-factor-only group (1.57%), although this did not reach statistical significance (p=0.0797). There was a noticeably higher event rate in the PAD group (18.54%), around double that for the CVD (8.29%) and CAD (10.07%) groups. These results mirror those reported for the registry as a whole and for the Western European population in the study.6
There is significant overlap between atherothrombotic disease in different locations, with 14.1% (85/601) of patients having disease in two or more locations. Moreover, analysis shows a statistically significant increase in the combined end point of CV death/MI/stroke plus hospitalisation (p=0.0043) with an increase in the number of symptomatic locations. The event rate for disease in a single vascular location almost doubled from 8.23% to 16.05% with two locations and a smaller incremental increase with three locations (18.30%). These results are in line with those reported for the whole registry (table 2).6

Discussion
From our previous paper, we know that the demographics of the UK REACH population are broadly similar to that of the Western European cohort.7 Despite the relatively small size of this UK cohort compared with the size of the overall registry, the results of this analysis of the one-year event rates mirrors that of the global study6 and further indicates that the results of REACH can be extrapolated to the UK situation (table 3).

The overall event rates for CV death/MI/stroke in the symptomatic population was 4.51% but the level of hospitalisations brought that figure up to about one in 10 patients (9.56%) in just one year. Further analysis by presenting disease showed that PAD contributed markedly to this rate and, indeed, had an event rate (including hospitalisations) around double that of CVD and CAD. Cardiovascular event rates and hospitalisations also increased with the number of symptomatic disease locations, underlining the high risk associated with multi-vascular disease. REACH has demonstrated that a significant proportion of individuals presenting with PAD, CVD or CAD will have disease in more than one vascular location and high rates of co-morbid illness such as hypertension, hypercholesterolaemia and diabetes; this emphasises the significant public health issue associated with atherothrombotic disease.
Both the global5–6 and the UK7 data show that although REACH is a contemporary registry with management according to current practice, a significant minority of patients with vascular disease are still not receiving adequate evidence-based treatments for CV risk factors (e.g. antiplatelets and lipid-lowering therapies), and fall short of targets for blood pressure, plasma cholesterol and non-smoking.6 This suggests that the undoubted healthcare burden of atherothrombosis, as demonstrated by REACH, could be substantially reduced with better risk factor management.
In summary, the one-year UK REACH data reflect that of Western Europe and the global cohort and underline the fact that, despite current use of evidence-based therapies, the event rates and hospitalisations associated with atherothrombosis remain high. This is particularly true for the multi-vascular patient and patients with PAD. More of our efforts need to be directed to ensure that the intensity of risk factor management is in line with the serious consequences of atherothrombotic disease revealed in the REACH registry.
Conflict of interest
JMM and GCK have served on advisory boards for, and received travel expenses, payment for speaking at meetings and support in attending national and international scientific meetings from, pharmaceutical companies, including Sanofi-Aventis and Bristol-Myers Squibb, the sponsors of the REACH Registry.
Collaborating Clinical Centres in the UK
Dr A Watt, Worcester Street, Stourbridge; Dr B King, Carterknowle Medical Centre, Sheffield; Dr DK Mistry, Paradise Medical Centre, Coventry; Prof R Donnelly, Derby City Hospital; Dr MJ Macleod, Aberdeen Royal Infirmary; Dr Bowen-Jones, Arrowe Park Hospital; Dr R Lal-Sarin, Wood End Health Centre, Coventry; Dr A Fuat, Carmel Medical Practice, Darlington; Prof S Homer Vanniasinkam, Leeds General Infirmary; Dr J Dwight, John Radcliffe Hospital, Oxford; Dr Baskaran, Parkway Health Centre, Croydon; Dr R Weir, Belgrave Medical Centre, Sheffield; Dr MB Addlestone, Halton, Leeds; Dr L Sherman, Bounds Green Group Practice, London; Dr D McKeith, Foxes Grove, Glasgow; Dr J Sharma, Mansfield Community Hospital; Dr JR Ferguson, Carrickfergus Health Centre, Belfast; Dr JR Courtney, Springhill Surgery, Bangor, Co Down; Dr W Thorburn, St Andrews Surgery, Keighley; Dr RP Agarwal, Old Swan Health Centre, Liverpool; Dr IR Parker, Comberton Surgery, Cambridge; Dr MJ Page and Partners, The Health Centre, Fleetwood; Dr M Singh, Brinsworth Medical Centre, Rotherham; Dr PS Lee & Partners, Armley Medical Practice, Leeds; Prof AH Barnett, Birmingham Heartlands Hospital; Dr JB Hamling, Oldfield Surgery, Bath; Dr SJ Morgan & Partners, Clifton Surgery, Cardiff; Dr SM Morgan, Four Elms Medical Centre, Cardiff; Dr Hole, Adcroft Surgery, Trowbridge; Dr TW Gietzen, Seaside Medical Centre, Eastbourne, Dr M James, Royal Devon & Exeter Hospital; Dr NH Patel, Southey Green Medical Centre, Sheffield; Dr P Husselbee, Highlands Surgery, Leigh on Sea; Dr C Mckinnon and Partners, Castlemilk Health Centre, Glasgow; Dr GDR Martin, Greenwood and Sneinton Medical Centre, Nottingham; Dr MG Kirby, The Surgery, Nevells Road, Letchworth; Prof C Shearman, Southampton General Hospital; Dr DPB Watson, Hamilton Medical Group, Aberdeen; Dr G Kassianos, Birch Hill Medical Centre, Bracknell; Dr RS Lawrence, West Byfleet Health Centre; Dr R Barker, Parishes Bridge Medical Practice, West Byfleet; Dr PJC Cummin & Partners, West Byfleet Medical Centre; Dr S Rowlands, Bradford Road, Trowbridge; Dr M Duckworth, Lovemead Group Practice, Trowbridge; Dr M Kent, West Road, Westcliff on Sea; Dr M Hughes, Eastview Surgery, Liverpool; Dr JP Kingsland, St Hilary Brow Group, Wallasey; Dr RA Cummins, Egremont Medical Centre, Wallasey; Dr A Brooks, Lister House Surgery, Derby; Dr PS Wiggins, Braidpark Drive, Glasgow; Dr BF Penney, Carmel Medical Practice, Darlington; Dr T Egerton, Priory Surgery, Belfast.
Key messages
- Atherothrombosis is the leading global cause of death and poses a significant health problem in the UK, where it is a government healthcare priority
- REACH is the largest global registry evaluating atherothrombotic risk, with over 68,000 patients in 44 countries
- The data for the UK, Western European and global REACH populations
are similar - The REACH Registry demonstrates that, despite a high use of evidence-based therapies, the rate of events and hospitalisations due to atherothrombosis remains high
- Notably, the event rates for peripheral arterial disease were higher than those in the coronary heart disease and cerebrovascular disease groups, and were significantly increased in those with multi-vascular disease
- It is time to take the diagnosis and management of atherothrombotic disease more seriously, in line with the high risk of cardiovascular events with which it is associated
References
- World Health Organization.
World health report. Making a difference. Geneva: World Health Organization, 1999. - World Health Organization. World health report. Shaping the future. Geneva: World Health Organization, 2003.
- Office for National Statistics. Health Survey for England 2004 – Updating of Trend Tables to Include 2004 Data. London: Health and Social Care
Information Centre, 2005. - Ohman EM, Bhatt DL, Steg PG et al. The REduction of Atherothrombosis for Continued Health (REACH) Registry: an international, prospective, observational investigation in subjects at risk for atherothrombotic events-study design. Am Heart J 2006;151:786.e1–786.e10.
- Bhatt DL, Steg PG, Ohman EM et al. International prevalence, recognition and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA 2006;295:180–9.
- Steg PG, Bhatt DL, Wilson PW et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA 2007;297:1197–206.
- Morrell JM, Kassianos GC. Baseline data from the UK arm of the REACH Registry. Br J Cardiol 2007;14:153–9.
