Spontaneous coronary artery dissection is a rare entity leading to acute coronary syndrome and sudden cardiac death. Most of these reported cases have occurred in young pregnant women and therapeutic management options are variable. We describe a case of a young patient who presented with ST-elevation myocardial infarction (STEMI) due to coronary artery dissection secondary to cocaine abuse.
Case history
A 24-year-old male security guard presented to the emergency department with residual central chest ache. The patient developed central, intense chest tightness radiating to the left shoulder four hours after taking 1 g of cocaine, and presented to our emergency room 12 hours later. He had no risk factors for atherosclerosis nor any prior collagen vascular disorders or autoimmune vasculitis. His electrocardiogram (ECG) revealed antero-lateral ST-elevation myocardial infarction (STEMI). He was haemodynamically stable with no evidence of left ventricular failure. Troponin-I was >50 IU (normal <0.03), with a normal baseline lipid profile and random blood glucose.
Primary percutaneous intervention was not considered due to late presentation and ECG evidence of completed infarct, as well as insignificant symptoms. In view of possible cocaine-induced vasospasm related antero-lateral STEMI, it was decided to manage the patient conservatively with nitrate infusion, diltiazem, dual antiplatelet and low molecular weight heparin (LMWH) after consultation with a specialist.
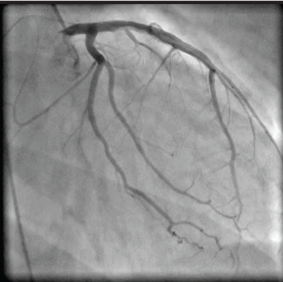
Echocardiogram later revealed a hypokinetic anterior wall and apex with reduced left ventricular function. Coronary angiography, on the second day, revealed a dissection extending from the proximal to mid segment of left anterior descending (LAD) coronary artery with normal left circumflex and right coronary arteries (figures 1 and 2). Left ventriculogram showed moderate left ventricular systolic dysfunction. His case was discussed at our local cardiology multi-disciplinary team (MDT) meeting and medical management was recommended due to the stable and asymptomatic nature. He was discharged on dual antiplatelet therapy and beta blockers with an appointment for cardiac magnetic resonance imaging (MRI), which confirmed extensive antero-apical infarction and moderate-to-severely impaired left ventricular systolic dysfunction (LVSD) with 10 non-viable and two viable segments.
Subsequently, he had two more admissions with chest pain and a small rise in troponin levels. His case was, therefore, re-discussed at our cardiology MDT meeting, where a decision to perform a repeat diagnostic coronary angiogram was suggested before any further intervention. Fortunately, his repeat coronary angiogram revealed spontaneously healed dissection.

Discussion
Spontaneous coronary artery dissection (SCAD) is a rare but recognised cause of non-atherosclerotic acute coronary syndrome. Pretty described the first case after a necropsy of a 42-year-old female with sudden death in 1931.1 Nearly 50 years later, the first angiographic report in a 55-year-old woman with acute myocardial infarction (AMI) was published.2 It is more common in women (3:1).3 One-fifth of women with SCAD present during pregnancy and 78% in the postpartum period, of which most present during the first two weeks.4 Spontaneous dissection of LAD is more common in women (87%), whereas right coronary artery spontaneous dissection is more common in males (67%).5 SCAD is also associated with pregnancy and postpartum,4,6 sleep deprivation,7 immunological disorders,8 antiphospholipid and anticardiolipin antibodies,9 collagen vascular disorders,10 vasculitis-like Kawasaki syndrome, oral contraceptive use,11 and intense physical activity.12
The first case of cocaine-induced SCAD due to right coronary artery dissection was described by Jaffe et al.13 in 1994. The second case of complete thrombotic occlusion due to dissection of LAD was reported by Steinhauer and Caulfield14 in 2001. Gelfand et al.15 reported the third case of dissection of the left main coronary artery extending distally to involve the left anterior descending and circumflex arteries in 2006. Our patient is the fourth case to our knowledge.
Cocaine-related cardiovascular effects are complex and multi-factorial. Its non-atherosclerotic effects are primarily due to its pro-adrenergic and sodium-channel blocking properties. Cocaine blocks the reuptake of presynaptic norepinephrine (noradrenaline) and dopamine, resulting in increased levels of these neurotransmitters and provoking a powerful sympathetic response due to sustained alpha- and beta-adrenergic stimulation. It also causes increased release of endothelin, which is a potent vasoconstrictor, and reduced production of nitric oxide, which is a potent vasodilator, resulting in profound vasoconstriction.16 Cocaine-related increased sympathetic discharge leads to high blood pressure and tachycardia, which translates into increased wall stress and work load resulting in increased oxygen demand.17 Cocaine has been shown to enhance platelet activation, adhesiveness and aggregation facilitating intra-coronary thrombosis.18 Thus, a combination of sympathetic over-activity, tachycardia, increased blood pressure, vasospasm and thrombosis, with the background of a possible diseased segment of arterial wall, may lead to abrupt sheer wall stress leading to dissection. Cocaine results in progressive atherosclerosis,19 with and without plaque formation, resulting in myocardial ischaemia and infarction.20 Hence, occlusion of the true lumen can occur if a dissected segment of the artery is displaced significantly. In our patient, we feel that all the above factors, except atherosclerosis, contributed to the spontaneous LAD dissection, although any underlying atherosclerosis cannot be excluded.
There is no standardised therapeutic management for patients with SCAD, as there are no studies comparing different modalities or any guidelines due to the small number of cases reported in the literature. In general, management should be individualised according to the patient’s clinical presentation, haemodynamic stability, the number of coronary arteries involved, site and extent of dissection, concomitant presence of atherosclerosis, and severity of spasm, within a MDT approach.
Role of thrombolysis in suspected cases of coronary artery dissection is controversial, as, theoretically, it can result in further progression of the dissection. Use of beta blocker, in cases of cocaine-induced dissection or AMI, should be deferred in the early stages as it can result in unopposed alpha-receptor induced vasoconstriction and tachycardia.21 Nitrates and calcium channel blockers can play a vital role in halting the progression of dissection.
Selected haemodynamically stable patients, and unstable patients or patients experiencing recurrent or persistent angina/ischaemia should be considered for urgent mechanical revascularisation. Percutaneous coronary intervention (PCI)22 could be opted for in selected patients, though it could be challenging due to wiring of false lumen and long stent use, with risk of late in-stent restenosis and thrombosis. Coronary artery bypass is preferred in patients with SCAD of left main stem or proximal LAD, failed PCI or when multiple coronary arteries are involved.23
Spontaneous healing of dissection, even in cases of multi-vessel involvement, has been reported.24 In our patient, a conservative approach was opted for initially as the patient was asymptomatic, haemodynamically stable, had a long dissected segment in mid to distal LAD, which appeared non-flow limiting, supplying an infarcted territory, and absence of underlying atherosclerotic changes with spontaneous recovery.
Conflict of interest
None declared.
Editors’ note
See also the editorial by Fletcher and Collinson on pages 102–3 of this issue.
References
- Pretty H. Dissecting aneurysm of coronary artery in a woman aged 42: rupture. BMJ 1931;1:667.
- Ciraulo DA, Chesen RB. Coronary arterial dissection. Chest 1978;73:677–9.
- Hamilos MI, Kochiadakis GE, Skalidis EI et al. Acute myocardial infarction in a patient with spontaneous coronary artery dissection. Hellenic J Cardiol 2003;44:348–51.
- Koul AK, Hollander G, Moskovits N, Frankel R, Herrera L, Shani J. Coronary artery dissection during pregnancy and the postpartum period: two case reports and review of literature. Cathet Cardiovasc Interv 2001;52:88–94.
- DeMaio SJ Jr, Kinsella SH, Silverman ME. Clinical course and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol 1989;64:471–4.
- Mather PJ, Hansen CL, Goldman B et al. Postpartum multivessel coronary dissection. J Heart Lung Transplant 1994;13:533–7.
- Suh SY, Kim JW, Choi CU et al. Complete angiographic resolution of spontaneous coronary artery dissection associated with sleep deprivation. Int J Cardiol 2007;119:e38–e39.
- Aldoboni AH, Hamza EA, Majdi K, Ngibzadhe M, Palasaidi F, Moayed DA. Spontaneous dissection of coronary artery treated by primary stenting as the first presentation of systemic lupus erythematosus. J Invasive Cardiol 2002;14:694–6.
- Reed RK, Malaiapan Y, Meredith IT. Spontaneous coronary artery dissection in a female with antiphospholipid syndrome. Heart Lung Circ 2007;16:120–2.
- Eltchaninoff H, Cribier A, Letac B. Peripheral and coronary dissection in a young woman. A rare case of type IV Ehler-Danlos syndrome. Arch Mal Coeur Vaiss 1997;90:841–4.
- Azam MN, Roberts DH, Logan WFWE. Spontaneous coronary artery dissection associated with oral contraceptive use. Int J Cardiol 1995;48:195–8.
- Ellis CY, Haywood GA, Monro JL. Spontaneous coronary artery dissection in a young woman resulting from an intense gymnasium “work out”. Int J Cardiol 1994;47:
193–4. - Jaffe BD, Broderick TM, Leier CV. Cocaine-induced coronary artery dissection. N Engl J Med 1994;330:510–11.
- Steinhauer JR, Caulfield JB. Spontaneous coronary artery dissection associated with cocaine use: a case report and brief review. Cardiovascular Pathology 2001;10:141–5.
- Eskander KE, Brass NS, Gelfand ET. Cocaine abuse and coronary artery dissection. Ann Thorac Surg 2001;71:340–1.
- Lange RA, Cigarroa RG, Yancy CW Jr et al. Cocaine-induced coronary-artery vasoconstriction. N Engl J Med 1989;321:1557–62.
- Benowitz NL. Clinical pharmacology and toxicology of cocaine. Pharmacol Toxicol 1993;72:3–12.
- Kugelmass AD, Oda A, Monahan K, Cabral C, Ware JA. Activation of platelets by cocaine. Circulation 1993;88:876–83.
- Hollander JE, Shih RD, Hoffman RS et al. Predictors of coronary artery disease in patients with cocaine-associated myocardial infarction. Cocaine-Associated Myocardial Infarction (CAMI) Study Group. Am J Med 1997;102:158–63.
- Weiss RJ. Recurrent myocardial infarction caused by cocaine abuse. Am Heart J 1986;111:793.
- Lange RA, Cigarroa RG, Flores ED et al. Potentiation of cocaine induced coronary vasoconstriction by beta adrenergic blockade. Ann Intern Med 1990;112:897–903.
- Vale PR, Baron DW. Coronary artery stenting for spontaneous coronary artery dissection: a case report and review of the literature. Cathet Cardiovasc Diagn 1998;45:280–6.
- Celik SK, Sagcan A, Altintig A et al. Primary spontaneous coronary artery dissections in atherosclerotic patients. Report of nine cases with review of the pertinent literature. Eur J Cardiothorac Surg 2001;20:573–6.
- Choi JW, Davidson CJ. Spontaneous multivessel coronary artery dissection in a long-distance runner successfully treated with oral antiplatelet therapy. J Invasive Cardiol 2002;14:675–8.
