Insights from the world of cardiology
Background
Statins are first choice for treatment of dyslipidaemia in both secondary and primary cardiovascular disease prevention. For every 1.0 mmol/L reduction in low-density lipoprotein cholesterol (LDL‑C), the risk of coronary heart disease (CHD) mortality decreases by 19% and overall mortality decreases by 12%.1 Despite statin treatment, a substantial number of cardiovascular events still occur, and one reason may be persistent lipid abnormalities including total cholesterol and LDL-C not at target, or low levels of high-density lipoprotein cholesterol (HDL-C) or elevated triglycerides. Results from the DYSlipidaemia International Study (DYSIS) in 22,063 statin-treated patients across 11 European countries and Canada, assessed the prevalence and types of persistent lipid abnormalities in patients receiving statin therapy, in both secondary and primary care settings.2 In this paper we report the UK results.
Methods
DYSIS was a multi-centre, cross-sectional, observational study of the lipid profile of statin-treated outpatients and the study design, methods and principal results are published.2 Outpatients under the care of a specialist or primary care physician were eligible for inclusion if they were ≥45 years old, had been receiving statin therapy for ≥3 months, and had ≥1 documented fasting blood lipid profile performed while on statins. Consecutive patients, fulfilling these inclusion criteria, who visited their specialist or primary care physician for whatever reason during a six‑month recruitment period were invited to participate. Routinely collected data from patient medical records were used, including the most recently recorded lipid parameters from the previous 6–12 months for total cholesterol, LDL-C, HDL‑C, and triglycerides.
Results
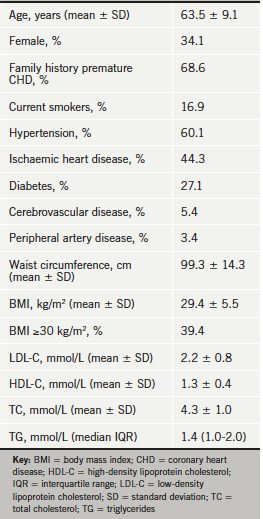
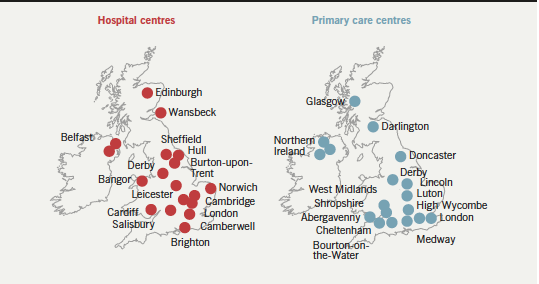
A total of 1,277 statin-treated patients with a clinical diagnosis of coronary or other atherosclerotic disease, or at high risk of developing cardiovascular disease (CVD), were recruited from 19 hospital and 19 primary care centres across the UK (figure 1).The patient characteristics are presented in table 1: 44.3% of patients had a history of coronary artery disease, 5.4% cerebrovascular disease and 3.4% peripheral artery disease.
Lipid-lowering treatment
All patients were taking a statin.
Lipid abnormalities
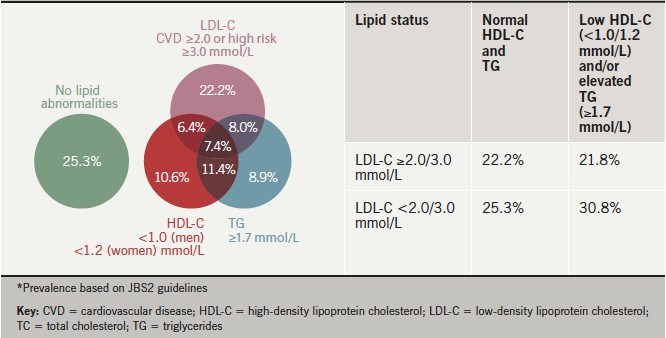
The distribution of single and combined lipid abnormalities in patients with a total lipid profile is shown in figure 2: 25.3% of patients had no lipid abnormalities and the rest had either an elevated LDL-C (≥2.0 mmol/L) or low HDL-C (<1.0 mmol/L men and <1.2 mmol/L women) or elevated fasting triglycerides (≥1.7 mmol/L) or a combination of these abnormalities. Overall, 56.1% of patients had LDL-C ≥2.0 mmol/L, 35.7% had low HDL-C and 35.6% had an elevated triglyceride level. In addition, 25.1% had a total cholesterol/HDL-C ratio ≥4.0. The proportion of patients at the total and LDL-C goals, the proportion with normal HDL-C and the proportion with normal triglycerides are shown in figure 3.

Discussion
Joint British Societies’ guidelines (JBS2) defined the same lipid targets for patients with atherosclerotic vascular disease, and those at high risk of developing CVD, namely a total cholesterol of <4.0 mmol/L and <2.0 mmol/L for LDL-C.3 The same targets for coronary patients were subsequently recommended by the National Institute for Health and Care Excellence (NICE) lipid guidelines, although not for primary prevention. Yet a majority of these coronary and high-risk patients, despite being actively treated with a statin, are not achieving these targets. In addition, a substantial minority also have either low HDL-C and/or elevated fasting triglycerides, further increasing cardiovascular risk.
In ASPIRE-2-PREVENT, 92.8% of coronary patients were taking a statin and, yet, 56.1% were above the LDL-C target of <2.0 mmol/L. In high-risk patients, only 61.2% were taking a statin and 74.8% were above the same LDL-C target.4 Therapeutic control in those taking a statin was also poor with only 44.7% of coronary patients below the LDL-C target, and 36.8% of high-risk patients for the same target.
In conclusion, these results continue to demonstrate the need for more intensive and comprehensive lipid management, especially of LDL-C, and where the target is not achieved with a high-intensity statin then combination lipid-lowering therapy should be considered. Other aspects of dyslipidaemia, including low HDL-C and elevated triglycerides, may also require a therapeutic strategy beyond statins, but this requires further evidence from randomised-controlled trials.
References
- Cholesterol Treatment Trialists’ (CTT) Collaboration. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet 2008;371:117–25. http://dx.doi.org/10.1016/S0140-6736(08)60104-X
- Gitt AK, Drexel H, Feely J et al. Persistent lipid abnormalities in statin-treated patients and predictors of LDL-cholesterol goal achievement in clinical practice in Europe and Canada. Eur J Prev Cardiol 2012;19:221–30. http://dx.doi.org/10.1177/1741826711400545
- British Cardiac Society, British Hypertension Society, Diabetes UK et al. JBS2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart 2005;91(suppl 5):v1–v52. http://dx.doi.org/10.1136/hrt.2005.079988
- Kotseva K, Jennings CS, Turner EL et al.; ASPIRE-2-PREVENT Study Group. ASPIRE-2-PREVENT: a survey of lifestyle, risk factor management and cardioprotective medication in patients with coronary heart disease and people at high risk of developing cardiovascular disease in the UK. Heart 2012;98:865–71. http://dx.doi.org/10.1136/heartjnl-2011-301603
