2. Assess lifestyle, comorbidities and willingness to change
See table 3.
3. Management
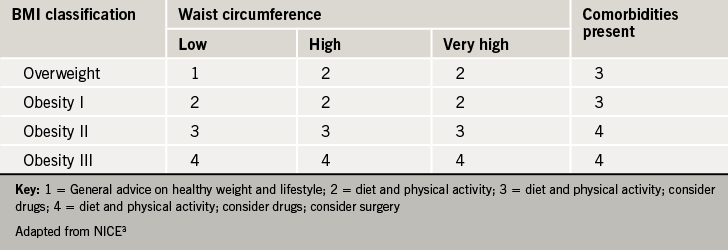
Interventions to encourage lifestyle change through increased physical activity, improved eating behaviour and healthy eating should be offered. Drug treatment should be considered where appropriate. The initial level of intervention to discuss can be guided by table 4.3 (More recent NICE guidance has given best practice guidance that these interventions should meet to motivate and support people making lifestyle changes).20
4. Consider recommendation of community services or referral
- For assessment of the underlying causes of overweight or obesity
- If a person has complex disease states
- If conventional treatment has failed
- If considering drug therapy for a person with a BMI > 50 kg/m2
- If specialist interventions may be needed
- If surgery is being considered
• How to accurately measure obesity – best practice tips
Opportunities to take these measurements include registration with a general practice, consultation for related conditions (such as type 2 diabetes and cardiovascular disease) and other routine health checks.
The following tips should ensure you can accurately measure and record height and weight, determine body mass index and accurately measure waist circumference.
Remember many people will be nervous about being measured and/or weighed. They may have had bad experiences of being weighed previously and some patients report that they avoid seeking advice about other medical problems because they feel so anxious about being weighed.
Height, weight and BMI
Click here for useful instructional videos on measuring patient height and weight
Make sure your surgery is equipped for treating people who are severely obese with, for example, special seating and adequate weighing and monitoring equipment.3 Create a positive environment to improve patients’ sense of acceptance. Ensure measurements are not hurried to ensure they are accurate as possible.
Before taking weight measurements, a person should remove their shoes, items in pockets and heavy clothing such as coats, belts and so on. Always measure weight without commenting on it in a private area.
When recording height, again make sure the person has removed shoes, caps and taken down any hairstyle or headwear on top of their head. Ensure their heels, hips, shoulders and head are flat against the wall. Ask them to take a deep breath and bring down measurement slide and record height. For certain groups of patients, such as those wearing turbans, those who cannot stand straight or steadily, or those who are wheelchair bound, height cannot be measured. It may be better to assess obesity using waist circumference measurements instead.
Once height and weight has been measured, BMI can be calculated using the following formula:
Weight (kg)
Height2 (m)
A useful patient resource for calculating BMI, provided by the BHF, can be found at http://www.bhf.org.uk/bmi/BMI_Calc.html
Waist circumference
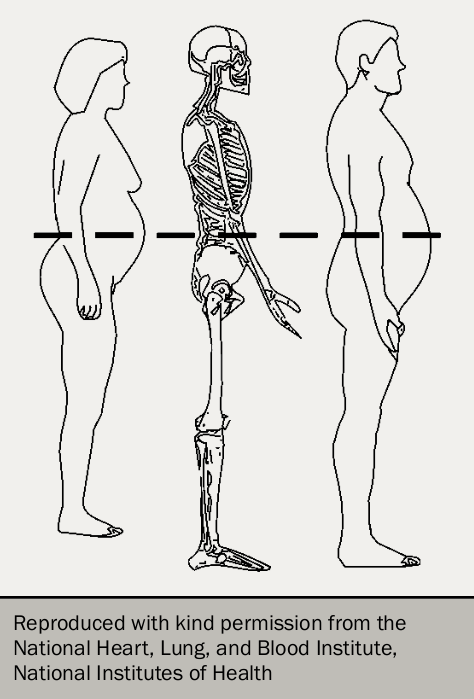
This is a good measure of ‘central obesity’ but does not help to assess people with a BMI > 35 kg/m2. Only one measurement is required per individual, and the cost of the equipment (a tape measure) is negligible.25 Figure 6 shows how to measure waist circumference.26
- Measure midway between the uppermost border of the iliac crest and the lower border of the costal margin
- Ensure you have a tape of adequate length available.
- Place tape around the abdomen at the level of this midway point, and take reading when the tape is snug but does not compress the skin (In may be difficult to accurately palpate those bony landmarks in very overweight patients in which case placing the tape at the level of the belly button is recommended24
- The least intrusive method for measuring waist circumference, which avoids bodily contact, is to ask the patient to hold the tape measure at the correct point and turn around 360 degrees.
Other guidance
The Scottish Intercollegiate Guidelines Network has produced guidance on the management of obesity (available in full here). The National Obesity Forum has also published guidelines on the management of adult obesity and overweight in primary care – available here. Guidance is also in development by the Royal College of General Practitioners.
Management
Assessment
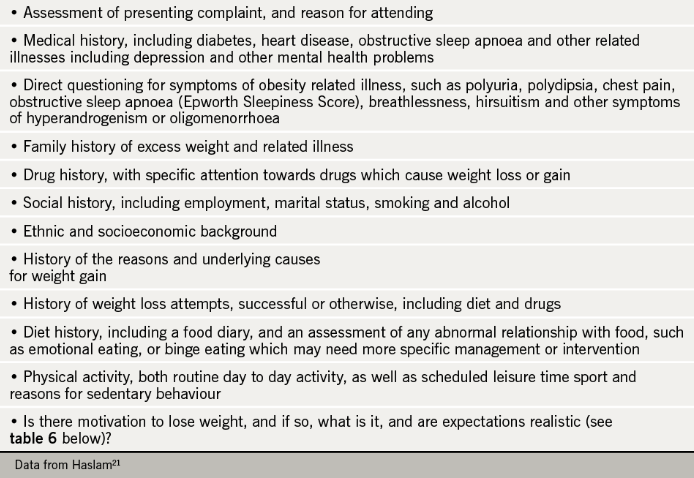
Screening for obesity-related comorbidities in primary care should be accompanied by assessment, examination, investigations and a full medical history (see table 5). The multifactorial nature of the condition including physical and mental health issues, ethnicity and deprivation should always be considered.21 Identify those with more complex needs who should be referred to more appropriate services (mental health, psychological etc).