Platelets
Platelets are small, anucleate, but highly complex cells, whose cytoskeleton, cell surface receptors and organelles all play vital roles in achieving haemostasis – roles which are becoming increasingly well understood. Produced by bone marrow megakaryocytes at a rate of around 1011 daily, platelets circulate in the blood in an inactive state. Upon activation – for example by vessel injury – they undergo a number of rapid changes leading to formation of a platelet plug and achievement of haemostasis, in collaboration with the coagulation cascade.
The membrane
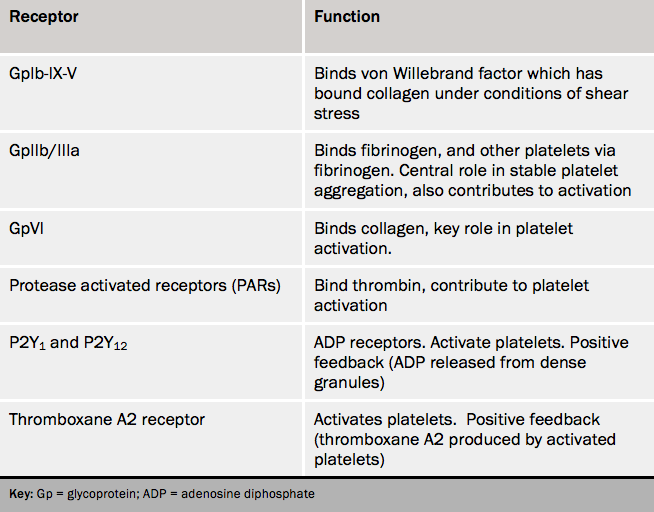
The major components of the platelet membrane are listed in table 4. Each can be bound by a specific ligand, and upon doing so a chain of actions is initiated that results in the adhesion and/or activation of the cell. The consequences of this are:
- shape change, from discoid to spherical, and the extrusion of pseudopodia, thus increasing surface area
- the increased expression of phospholipids and phosphatidylserine, thus providing the optimum surface for the assembly of components of the coagulation cascade
- granule release, resulting in the extrusion of a larger number of biologically active mediators, and the appearance of further adhesion molecules, increasing platelet–platelet adhesion and platelet–subendothelial adhesion.
The cytoplasm
The major organelles participating directly in thrombosis are dense bodies and alpha granules. These granules are released upon platelet activation, and can be best thought of as promoting further platelet recruitment through positive feedback, while also promoting coagulation locally. The contents of dense bodies include serotonin (5-hydroxytryptamine), adenosine triphosphate (ATP), adenosine diphosphate (ADP) and calcium. Alpha granules contain a huge variety of mediators including:
• components of the coagulation cascade (fibrinogen, von Willebrand factor and factor V)
• molecules involved in fibrinolysis and repair (plasminogen, PAI-1, platelet derived growth factor)
• chemokines for leucocyte recruitment (platelet factor 4, beta-thromboglobulin) and
• promoters of further platelet aggregation (thrombospondin and fibronectin).
Fusion of alpha granules with the platelet membrane also increases membrane concentrations of receptors involved in platelet adhesion, such as P-selectin and GpIIb/IIIa.
As well as granule release, activated platelets generate thromboxane A2 from membrane phospholipids via the enzyme cyclooxygenase. Thromboxane A2 further augments platelet activation. The importance of its role is highlighted by the effectiveness of the cyclooxygenase inhibitor aspirin in reducing platelet function.
