Other agents
Vorapaxar
Vorapaxar is a first in class oral inhibitor of the platelet thrombin receptor PAR-1. Its place in therapy is currently uncertain as trials to date have showed modest benefits in reducing ischaemic events, with substantial risks of haemorrhage, especially intracranial haemorrhage.29
Iloprost
Iloprost is a prostacyclin analogue that exerts its effects by promoting vasodilatation and inhibiting ADP-induced platelet aggregation, thereby opposing the effects of thromboxane A2. It may also increase the rate of metabolism of tissue plasminogen activator by the liver, but must be continuously infused.
Cilostazol
Cilostazol, like dipyridamole, is a phosphodiesterase inhibitor and so reduces platelet aggregation but also increases arterial vasodilation. Its use is restricted to those with intermittent claudication, in peripheral arterial disease patients.
Summary
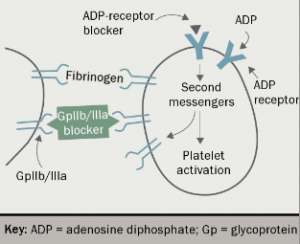
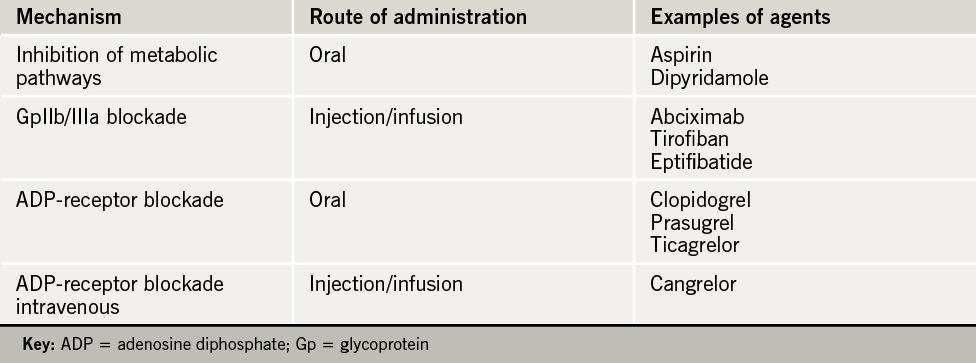
Established antiplatelet agents are summarised in table 1, while figure 4 illustrates how our knowledge of platelet physiology has enabled us to inhibit its activity.
Haemorrhage
The British Committee for Standards in Haematology (BCSH) issued recent guidelines on the management of bleeding in patients taking antithrombotic agents.1 Simply stopping the agent may not be sufficient if bleeding is severe, as it may take several days for platelet function to return to normal (see table 2).

Options to stop bleeding range from basic haemostatic measures (pressure, surgical opinion) to platelet transfusion. Decisions regarding stopping/reversing antithrombotic agents have clear implications for thrombotic risk; specialist advice should be sought.
close window and return to take test
References
1. Makris M, Van Veen J J, Tait C R, Mumford A D, Laffan M. Guideline on the management of bleeding in patients on antithrombotic agents. Br J Haematol 2013:160: 35–46. http://dx.doi.org/10.1111/bjh.12107
2. Harrison P, Mackie I, Mumford A et al. and British Committee for Standards in Haematology. Guidelines for the laboratory investigation of heritable disorders of platelet function. Br J Haematol 2011;155: 30–44. http://dx.doi.org/10.1111/j.1365-2141.2011.08793.x
3. Antiplatelet trialists collaboration. Collaborative overview of randomised trials of antiplatelet therapy I: prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ 1994;308:81–106. Erratum in: BMJ 1994;308:1540. http://dx.doi.org/10.1136/bmj.308.6921.81
4. Dretzke J, Riley R, Lordkipanidzé M et al. The prognostic utility of tests of platelet function for the detection of ‘aspirin resistance’ in patients with established cardiovascular or cerebrovascular disease: a systematic review and economic evaluation. Health Technol Assess 2015;19:1–366. http://dx.doi.org/10.3310/hta19370
5. Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR. Aspirin “resistance” and risk of cardiovascular morbidity: systematic review and meta-analysis. BMJ 2008;336:195–8. http://dx.doi.org/10.1136/bmj.39430.529549.BE
6. National Institute for Health and Care Excellence. CG 172. MI – secondary prevention: secondary prevention in primary and secondary care for patients following a myocardial infarction. London: NICE 2013 (accessed 8.9.2015).
7. National Institute for Health and Care Excellence. Clinical Knowledge Summaries: antiplatelet treatment. London: NICE, http://cks.nice.org.uk/antiplatelet-treatment#!topicsummary (accessed 8.9.2015).
8. Belch J, MacCuish A, Campbell I, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ 2008;337:a1840. http://dx.doi.org/10.1136/bmj.a1840
9. National Institute of Health and Care Excellence. CG180. Atrial fibrillation: the management of atrial fibrillation. London: NICE 2014 (accessed 8.9.2015).
10. Camm AJ, Lip GYH, De Caterina R et al. 2012 focused update of the ESC guidelines for the management of patients with atrial fibrillation. Eur Heart J 2012;33:2719–47. http://dx.doi.org/10.1093/eurheartj/ehs253
11. National Institute of Health and Care Excellence. Technology appraisal guidance [TA210]. Clopidogrel and modified-release dipyridamole for the prevention of occlusive vascular events. London: NICE 2010 (accessed 9.9.2015).
12. National Clinical Guidelines for Stroke, prepared by the Intercollegiate Stroke Working Party. Royal College of Physicians, 2012.
13. CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet 1996;348:1329–39. http://dx.doi.org/10.1016/S0140-6736(96)09457-3
14. Mehta SR, Yusuf S, Peters RJ, et al. for the clopidogrel in unstable angina to prevent recurrent events trial (CURE) investigators. Effects of pre treatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 2001;358:527–33. http://dx.doi.org/10.1016/S0140-6736(01)05701-4
15. Belch JJ, Dormandy J; CASPAR writing committee. Results of the randomized, placebo-controlled clopidogrel and acetylsalicylic acid in bypass surgery for peripheral arterial disease (CASPAR) trial. J Vasc Surg 2010;52:825–33. http://dx.doi.org/10.1016/j.jvs.2010.04.027
16. Mehta SR, Tanguay JF, Eikelboom JW et al. Double-dose versus standard-dose clopidogrel and high-dose versus low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomised factorial trial. Lancet 2010;376:1233–43. http://dx.doi.org/10.1016/S0140-6736(10)61088-4
17. Bauer T, Bouman HJ, van Werkum JW, Ford NF, ten Berg JM, Taubert D. Impact of CYP2C19 variant genotypes on clinical efficacy of antiplatelet treatment with clopidogrel: systematic review and meta-analysis. BMJ 2011;343:d4588. http://dx.doi.org/10.1136/bmj.d4588
18. Tantry U, Bonello L, Aradi D et al. Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol 2013;62:2261–73. http://dx.doi.org/10.1016/j.jacc.2013.07.101
19. Cardoso RN, Benjo AM, DiNicolantonio JJ et al. Incidence of cardiovascular events and gastrointestinal bleeding in patients receiving clopidogrel with and without proton pump inhibitors: an updated meta-analysis. Open Heart 2015;2(1):e000248. http://dx.doi.org/10.1136/openhrt-2015-000248
20. Saboureta P, Taiel-Sartral M. New antiplatelet agents in the treatment of acute coronary syndromes. Arch Cardiovasc Dis 2014:107:178–87. http://dx.doi.org/10.1016/j.acvd.2014.01.009
21. Wiviott SD, Braunwald E, McCabe CH, et al. for the TRITON-TIMI 38 investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007;357:2001–15. http://dx.doi.org/10.1056/NEJMoa0706482
22. Roe MT, Armstrong PW, Fox KA, et al. for the TRILOGY ACS investigators. Prasugrel versus clopidogrel for acute coronary syndromes without revascularization. N Engl J Med 2012;367:1297–309. http://dx.doi.org/10.1056/NEJMoa1205512
23. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2009;361:1045–57. http://dx.doi.org/10.1056/NEJMoa0904327
24. Steg P, Bhatt D, Hamm C, et al. Effect of cangrelor on periprocedural outcomes in percutaneous coronary interventions: a pooled analysis of patient-level data. Lancet 2013;382:1981–92. http://dx.doi.org/10.1016/S0140-6736(13)61615-3
25. Aradi D, Storey R, Komócsi A, et al. Expert position paper on the role of platelet function testing in patients undergoing percutaneous coronary intervention. Eur Heart J 2014;35:209–15. http://dx.doi.org/10.1093/eurheartj/eht375
26. Trenk D, Stone GW, Gawaz M, et al. A randomized trial of prasugrel versus clopidogrel in patients with high platelet reactivity on clopidogrel after elective percutaneous coronary intervention with implantation of drug-eluting stents: results of the TRIGGER-PCI (Testing Platelet Reactivity in Patients Undergoing Elective Stent Placement on Clopidogrel to Guide Alternative Therapy With Prasugrel) study. J Am Coll Cardiol 2012;59:2159–64. http://dx.doi.org/10.1016/j.jacc.2012.02.026
27. National Institute for Health and Care Excellence. Technology appraisal guidance TA182. Prasugrel for the treatment of acute coronary syndromes with percutaneous coronary intervention. London: NICE, October 2009. http://guidance.nice.org.uk/TA182/Guidance/pdf/English
28. National Institute for Health and Care Excellence. Technology appraisal guidance TA236. Ticagrelor for the treatment of acute coronary syndromes. London: NICE, October 2011. http://www.nice.org.uk/ta236
29. Roffi M, Patrono C, Collet J, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2015;pii: [Epub ahead of print]. http://dx.doi.org/10.1093/eurheartj/ehv320
30. Steg PG, James SK, Atar D et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J 2012;33:2569–619. http://dx.doi.org/10.1093/eurheartj/ehs215
31. National Institute of Health and Care Excellence. CG94. Unstable angina and NSTEMI: the early management of unstable angina and non-ST-segment-elevation myocardial infarction. London: NICE, 2010 (accessed 13.9.2015).
Further reading
Sharma RK, Voelker DJ, Sharma R, Reddy HK, Dod H, Marsh JD. Evolving role of platelet function testing in coronary artery interventions. Vasc Health Risk Manag 2012;8:65–75. http://dx.doi.org/10.2147/VHRM.S28090
Michelson AD. Advances in antiplatelet therapy. Hematology Am Soc Hematol Educ Program 2011;2011:62–9. http://dx.doi.org/10.1182/asheducation-2011.1.62
Gasparyan AY. Aspirin and clopidogrel resistance: methodological challenges and opportunities. Vasc Health Risk Manag 2010;6:109–12. http://dx.doi.org/10.2147/VHRM.S9087
National Institute for Health and Clinical Excellence. CG48. Secondary prevention in primary and secondary care for patients following a myocardial infarction. London: NICE, May 2007. Available from: http://guidance.nice.org.uk/CG48
Breet NJ, van Werkum JW, Bouman HJ et al. Comparison of platelet function tests in predicting clinical outcome in patients undergoing coronary stent implantation. JAMA 2010;303:754–62. Erratum in: JAMA 2010;303:1257. http://dx.doi.org/10.1001/jama.2010.181
Hicks T, Stewart F, Eisinga A. NOACs versus warfarin for stroke prevention in patients with AF: a systematic review and meta-analysis. Open Heart 2016;3:e000279. http://dx.doi.org/10.1136/openhrt-2015-000279
See also www.bnf.org
close window and return to take test
All rights reserved. No part of this programme may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the publishers, Medinews (Cardiology) Limited.
It shall not, by way of trade or otherwise, be lent, re-sold, hired or otherwise circulated without the publisher’s prior consent.
Medical knowledge is constantly changing. As new information becomes available, changes in treatment, procedures, equipment and the use of drugs becomes necessary. The editors/authors/contributors and the publishers have taken care to ensure that the information given in this text is accurate and up to date. Readers are strongly advised to confirm that the information, especially with regard to drug usage, complies with the latest legislation and standards of practice.
Healthcare professionals should consult up-to-date Prescribing Information and the full Summary of Product Characteristics available from the manufacturers before prescribing any product. Medinews (Cardiology) Limited cannot accept responsibility for any errors in prescribing which may occur.
