Delivery methods
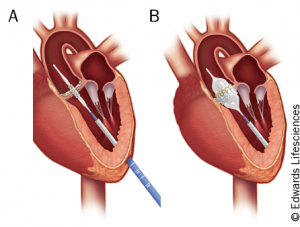
The most common approach is transfemoral (see figure 2). Although general anaesthesia is still usually used, this approach is feasible without general anaesthesia, which is an advantage for these high-risk patients.4

The transapical approach (see figure 3) is necessary if there is poor femoral artery access due to atherosclerosis, small vessel diameter, or extreme tortuosity,5 or in patients with heavily calcified aortas in which there is increased risk of emboli from manipulation by the larger diameter catheters used in the transfemoral approach. A left anterolateral minithoracotomy in the fifth intercostal space is created for access to the left ventricular apex. Next, a guidewire is passed through the apex and into the ascending aorta, and finally the prosthesis is delivered antegrade onto the stenotic valve.6
Less frequently a subclavian or direct aortic approach is made. The aortic approach is via a small right-upper “J” hemisternotomy or a small right-anterior thoracotomy. These allow direct insertion of a guidewire into the ascending aorta, allowing a catheter to deploy the prosthesis onto the diseased native valve. Operators find this implantation method to be easier and more accurate, yet the disadvantage is the increased invasiveness and the need for general anaesthetic.5 For all three methods, fluoroscopy plus transoesophageal echocardiography are used for positioning the valves.
Figure 4 shows a TAVI procedure via transaortic approach, performed by Mr Vinyak Bapat, Consultant Cardiac Surgeon, Dr Martyn Thomas, Consultant Interventional Cardiologist, and Dr Jane Hancock, Consultant Cardiologist/Imaging Specialist (St Thomas’ Hospital, London).
Models
There are now three TAVI devices commonly available in the UK:
- balloon-expandable Sapien™ (Edwards Lifesciences)
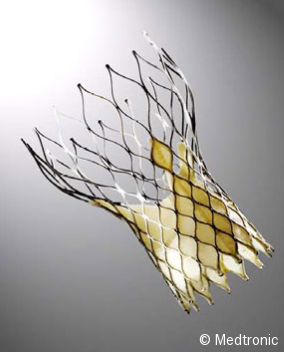
- self-expanding Corevalve™ (Medtronic)
- Portico™ (St Jude Medical).
The SapienTM is composed of bovine pericardial cusps within a balloon-expandable, stainless-steel or cobalt-chromium stent. It is currently available in four sizes, between 23 and 29 mm. When implanted, the mid-point of the valve lies approximately at the level of the aortic valve so they can be placed above a subaortic septal bulge and are not dependent on the size of the aorta above the annulus. Precise deployment is crucial since a deviation in position can result in the prosthetic valve embolising into the left ventricle or distal aorta.9
The CoreValveTM (see figure 5) is composed of porcine pericardial tissue within a self-expanding nitinol stent. It is anchored at the native valve as well as the ascending aorta, which may allow for easier positioning.10 The Portico™ (see figure 6) is composed of porcine pericardial tissue within a self-expanding nitinol stent.
During valve deployment, rapid ventricular pacing is required to temporarily decrease cardiac output for deploying balloon-expandable valves, but not necessarily needed for self-expanding models.11 Although uncommon, displacement of a heavily calcified cusp can obstruct coronary flow. The longstanding effects of the metallic components of the prosthetic devices are unknown.