What is pulmonary hypertension? Definition and clinical classification
Pulmonary hypertension (PH) is a condition that may be defined as an increase in mean pulmonary arterial pressure (PAP) ≥25 mmHg at rest as assessed by cardiac catheterisation. The normal PAP at rest is 14 mmHg, with an upper limit of normal of approximately 20 mmHg (ESC guidelines).1 Patients with mean PAP between 21 and 24 mmHg are in a grey area where outcome is unknown. When confronted with a patient with borderline PH, it is important to decide how clinically important the PH is. There is no definition of PH on exercise since there are insufficient data to provide a definition.
Furthermore, pulmonary arterial hypertension (PAH), characterised by the presence of pre-capillary PH, is defined haemodynamically by the presence of a pulmonary artery wedge pressure (PAWP) of ≤15 mmHg and a pulmonary vascular resistance (PVR) of >3 Wood units, in the absence of other causes (see table 1).
Table 1. Haemodynamic definitions of pulmonary hypertension
This can be viewed as table 3 in 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension
Post capillary PH, for example, PH due to left heart disease, is defined haemodynamically with various combinations of PAP, PAWP, cardiac output (CO), diastolic pressure gradient (DPG) and PVR, as shown in table 1.
When to refer
In general, the referral criteria to send a patient to a PH centre indicate that this is better done sooner rather than later. Some forms of PH may deteriorate rapidly or may be associated with important symptoms at the time that the diagnosis is suspected. Data from the placebo arms of randomised clinical trials have shown that patients with PAH may deteriorate very significantly over three months and patients with severe symptoms may die within this time.
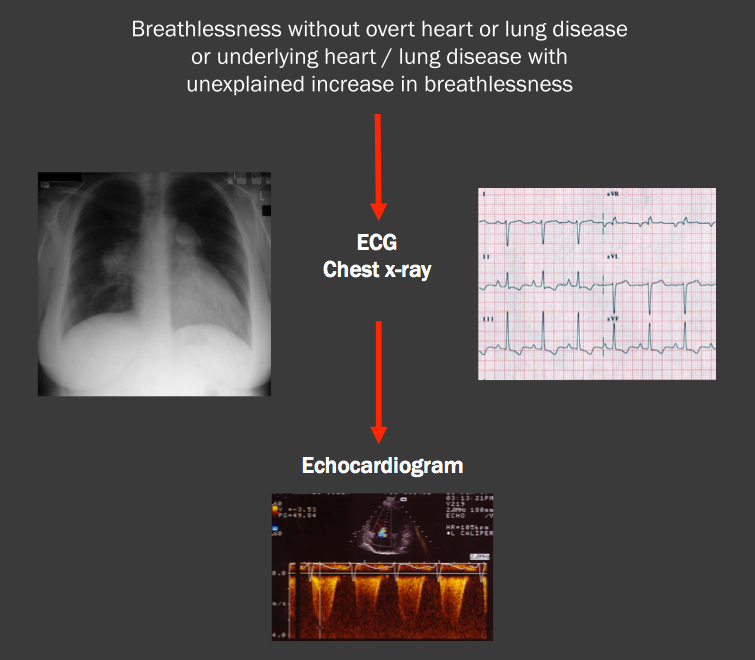
Patients should be referred to a designated centre (listed in module 2 of this programme) when investigations suggest the diagnosis (see figure 1). Adults with pulmonary hypertension should be referred when the following diagnoses are suspected or proven:
- PAH
- chronic thromboembolic and/or embolic disease
- miscellaneous causes.
Referral should be considered in cases of PH in hypoxic lung disease or cardiac disease, but only if symptoms or estimated PASP at echocardiography seems excessive (>60 mm Hg) or the patient has another disease which may be associated with PAH.
The following procedures should be carried out in adults before referral:
- routine blood tests
- ECG
- chest x ray
- transthoracic echocardiogram
- spirometry.
If possible, all patients should be seen by a consultant in cardiology or respiratory medicine before referral to a designated centre. Patients with PH may deteriorate rapidly. It is important that referrals are not delayed in order to undertake more extensive investigation if it is clear that PH is the dominant problem. PH centres undertake a package of investigations over a short period of time, and the results are reviewed at a multidisciplinary team meeting to establish the diagnosis and start appropriate treatment promptly. Patients under the age of 16 should be referred to the PH centre for children.2
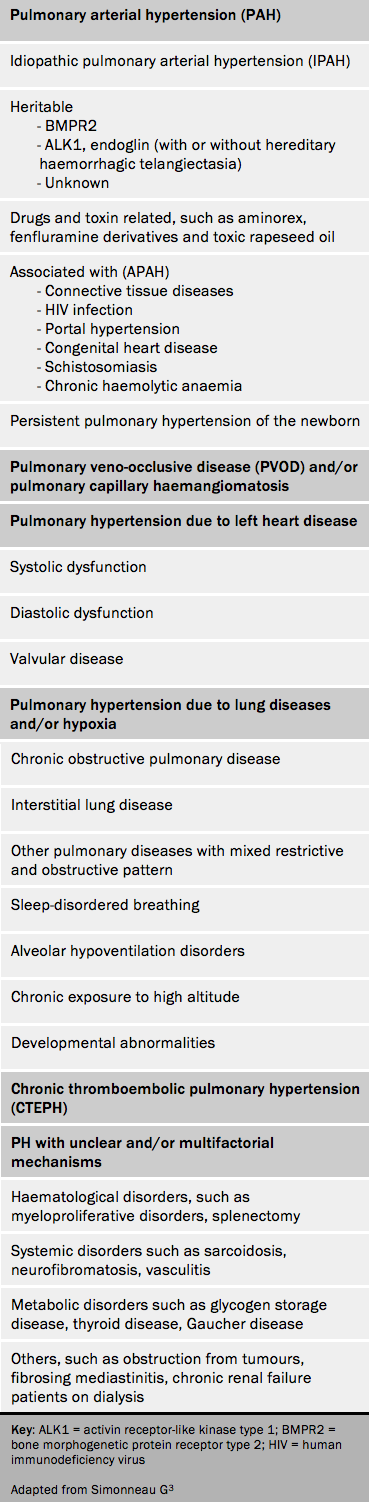
PH has many diverse causes. The purpose of the clinical classification is to identify patients who have similarities in pathophysiology of PH, clinical presentation and to help guide treatment. Note that the natural history of PH may vary widely within the main groups of the classification. The most recent version of the clinical classification, from the 2015 ESC/ERS guidelines, is shown in table 2.3
The clinical classification should be used to determine the precise cause of PH in each patient. Some patients may have several causes of PH but it is important in an individual to determine the most important cause. The clinical classification is arrived at by taking a detailed history to cover potential causes of PH relevant to the patient, including a two-generation family history and specific investigations. It is important to be clear about the cause of pulmonary hypertension: the haemodynamic changes may be similar across the different groups but the groups differ considerably in both treatment approaches and prognosis. As an example, a thorough work-up will identify the comparatively small number of patients for whom surgical treatment is curative.
The clinical classification of PAH associated with congenital heart disease (CHD) is reported in table 2.1 Patients with congenital heart disease should always be managed in association with an adult congenital heart disease clinic since PH may not be their most important cardiovascular disease problem and treatment may extend to intervention or surgery for the congenital heart disease itself. Note that in Eisenmenger’s syndrome there is multiple organ involvement and attention needs to be paid to other important medical issues in these patients such as iron status. Therapeutic venesection should be avoided.
See table 6 in 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension
