Heart failure rates
Heart failure has a profound impact on the lives of patients and their carers. It is costly to manage as patients often need hospital admissions for medical care and may require expensive device-based therapy.
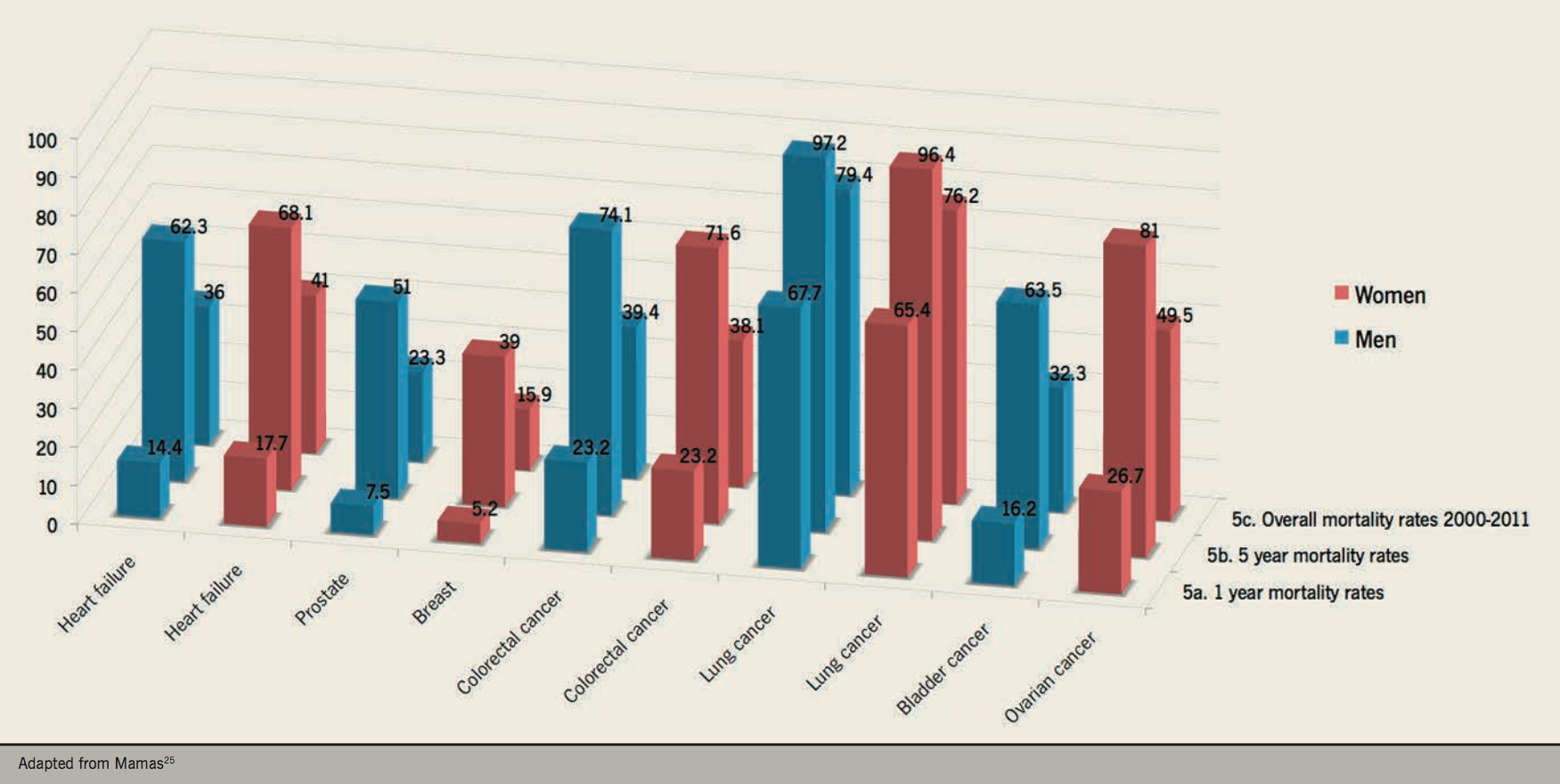
Despite advances in management, heart failure prognosis remains poor. A recent epidemiological study of 56,658 patients registered at general practices in Scotland found heart failure mortality rates one year after diagnosis of 14.4% for men and 17.7% for women (figure 5) and five-year mortality rates of 62.3% and 68.1% respectively (figure 5). Overall mortality rates for heart failure were similar to that of colorectal cancer and worse than those for bladder, prostate and breast cancer during the 11-year study period from 2000 to 2011 (figure 5).25
National Heart Failure Audit
The National Heart Failure Audit 2015–16 found the mean age of patients admitted with acute heart failure was 78 years. The in-patient mortality rate was 8.9%. Patients over 75 years are more than twice as likely to die as an in-patient (11.0%) than younger patients (4.5%). Of those who survived to discharge, 6.0% had died within 30 days and 35.3% had died before one year.2
All patients admitted with heart failure received an electrocardiogram (ECG), and 90% had an imaging test of heart function, usually an echocardiogram (echo). Most patients (68.3%) had left ventricular systolic dysfunction (LVSD); 34.8% of patients were diagnosed with valve disease, 11.1% with diastolic dysfunction and 7.1% with left ventricular hypertrophy. These diagnoses are not mutually exclusive. Women and older patients were less likely to have LVSD to explain their heart failure.2
The audit does not record the availability and use of natriuretic peptide measurements, which is probably now the best diagnostic tool for heart failure. Details of natriuretic peptides can be found in module 2: diagnosis.
Place of care is also important: the death rate for patients treated on cardiology wards (6.6%) is lower than for those admitted to general medical wards (9.7%) or other wards (11.5%). Of those receiving no specialist input, in-hospital mortality was 12.6% compared to 7.8% among those who received care from a consultant cardiologist, a consultant with an interest in heart failure or heart failure specialist nurse.
Approximately 80% of all patients admitted with heart failure will receive some in-patient specialist input from a consultant cardiologist, a heart failure nurse specialist or consultant physician with an interest in heart failure. An important observation is that patients receiving specialist care have a longer duration of stay than those who do not, perhaps reflected in their greater likelihood of receiving optimal treatment (which might be expected to translate into better outcome and fewer re-hospitalisations).2
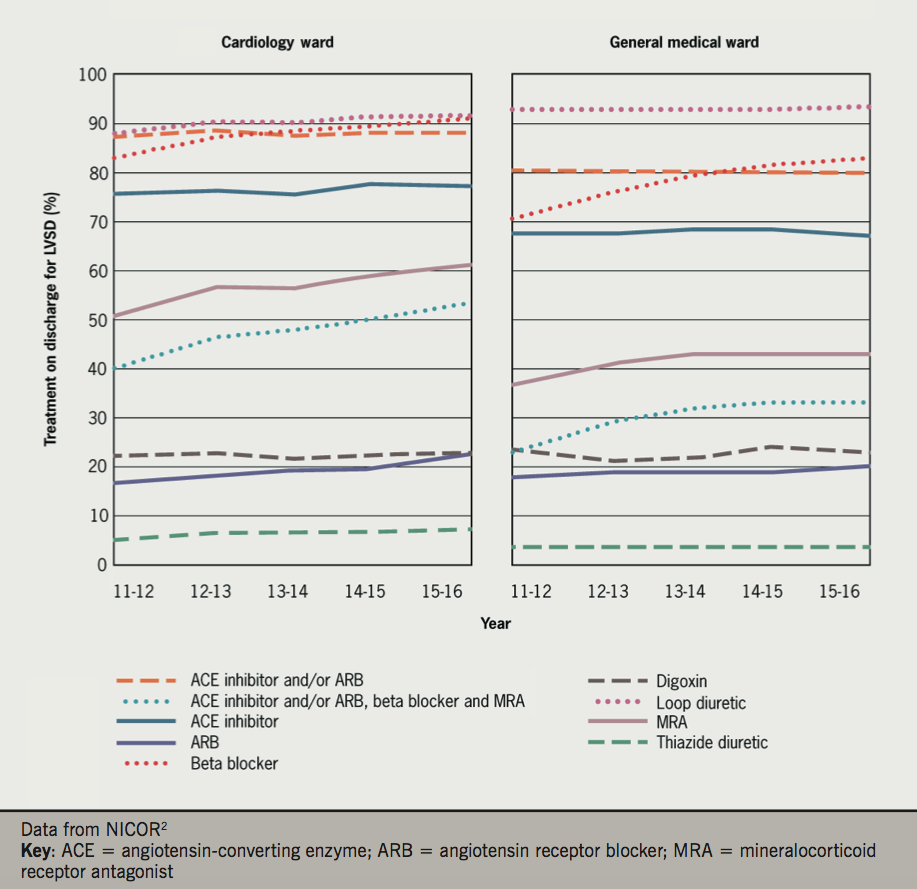
For example, 45% of patients treated for LVSD on a cardiology ward were taking ‘triple therapy’ (angiotensin converting enzyme [ACE] inhibitor or angiotensin receptor blocker [ARB], beta blocker and mineralocorticoid receptor antagonist [MRA]) on discharge compared to 21% on other medical wards.
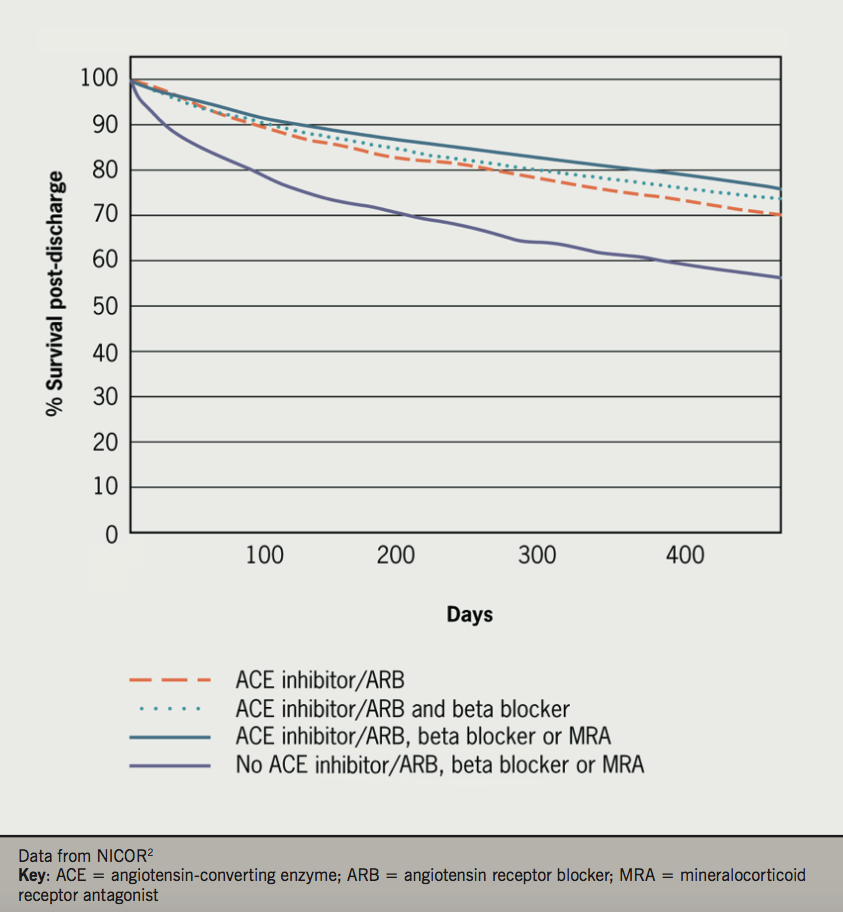
The use of beta blockers, ACE inhibitors and MRAs, i.e. spironolactone/eplerenone, together and separately, were all associated with better survival. Conversely the use of loop diuretics at discharge was associated with worse survival (figure 6).2 While rates of ACE inhibitor prescription on discharge have remained stable since 2009, there has been an increase in the rates of beta blocker and MRA prescriptions on discharge.
For the first time, the heart failure audit 2015–16 has found a significant reduction in the number of in-patient deaths (8.9% versus 9.6% in 2014–15). The rate of prescription of triple therapy medications has increased on cardiology and general medical wards: better treatment has led to better outcomes.
However, there was significant variability in mortality rates between hospitals: place of care still affects mortality rate (figure 7). More work is required to ensure that patients with heart failure receive a more consistent service at both a local and nationwide level.

All rights reserved. No part of this programme may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the publishers, Medinews (Cardiology) Limited.
It shall not, by way of trade or otherwise, be lent, re-sold, hired or otherwise circulated without the publisher’s prior consent.
Medical knowledge is constantly changing. As new information becomes available, changes in treatment, procedures, equipment and the use of drugs becomes necessary. The editors/authors/contributors and the publishers have taken care to ensure that the information given in this text is accurate and up to date. Readers are strongly advised to confirm that the information, especially with regard to drug usage, complies with the latest legislation and standards of practice.
Healthcare professionals should consult up-to-date Prescribing Information and the full Summary of Product Characteristics available from the manufacturers before prescribing any product. Medinews (Cardiology) Limited cannot accept responsibility for any errors in prescribing which may occur.