Why do we calculate risk?
The purpose of a public health intervention is to take broad measures that can improve the well-being and general health of as many people as possible in the most cost-effective way. This can work well when, for example, the solution is based on engineering (such as installing improved sewers and waste treatment plants), but it is more complex when it involves giving medical treatments to an individual. All drugs carry the risk of side effects and therefore, there is a potential risk to the patient. Drug cost is also an important consideration. Where the risk and cost of the drug is extremely low, it may be applied to the entire population as, for example, with the fluoridation of water to prevent dental caries, but for most drugs, there must be an element of rationing.
While the role of public health is to improve the health of the whole population, the physician’s role is to treat their patient as an individual. This leads to the obvious tension that preventative drug treatment may be offered to those who may not benefit enough to meet cost-efficiency parameters. There is also the possibility that someone’s risk may be atypical for their age and therefore the potential that they may benefit from treatment may not be identified without a formal risk assessment process. Except for certain specific groups, risk is calculated to allow us to target those individuals who are most likely to benefit whilst avoiding treating those whose potential benefit is insufficient.
Who is at risk?
Essentially, everyone is at risk of every sort of disease. What is important is identifying who is most at risk and who exceeds the threshold above which treatment is worthwhile.
Cardiovascular disease (CVD), the primary focus of this module, is one of the leading causes of death in the UK. Approximately 27% of deaths (175,000 per year) are caused by heart and circulatory disease and 7.6 million people are living with CVD.1 This sounds bad but in the last 50 years, the death rate from CVD has declined by approximately 75%, which clearly demonstrates that our current treatment approach is working.
The main risk factors of interest include: (in alphabetical order) age, blood pressure, diabetes, ethnicity, family history, gender, lipids, obesity and smoking. This information has been derived from many epidemiological studies.
The seminal study was the Framingham Heart Study,2 which began in 1948 and continues today. It started by recruiting 5,209 men and women between the ages of 30 and 62 years from the town of Framingham and carried out detailed physical examinations and pathology testing every two years. A second-generation study recruited 5,124 extra participants in 1971. In 1994, a newer, more ethnically diverse population was recruited for the first Omni-cohort group. In 2002, the grandchildren of the original cohort were recruited to another study and in 2003, a second Omni-cohort was enrolled. Since then, a new offspring cohort has also been enrolled. In 2023, the Framingham Heart Study celebrated 75 years of research and there are now 15,447 people enrolled in the study.3
Table 1. Main risk factors for CVD
| Major risk factors |
|---|
| Age |
| Gender (male) |
| Smoking |
| High blood pressure |
| Increased total cholesterol |
| Increased LDL cholesterol level |
| Decreased HDL cholesterol level |
| Diabetes mellitus |
| Left ventricular hypertrophy (identified in resting ECG) |
| Pre-disposing risk factors |
| Overweight and obesity (especially truncal / abdominal obesity) |
| Physical inactivity |
| Family history of CVD |
| Socioeconomic factors (deprivation etc.) |
| Ethnicity (South Asian) |
| Psychosocial factors |
| Systemic inflammatory diseases (e.g. rheumatoid arthritis, systemic lupus erythematosus) |
| Additional risk factors |
| Triglycerides |
| Lipoprotein(a) |
| Key: CVD = cardiovascular disease; ECG = electrocardiogram; HDL = high-density lipoprotein; LDL = low-density lipoprotein |
Other important risk factor identification studies include INTERHEART (Effect of Potentially Modifiable Risk Factors Associated with Myocardial Infarction),4 the London Bus Driver Study,5 the Whitehall studies6 and many others. These identified the major risk factors associated with CVD listed in table 1.
How can we interpret risk factors?
Interpreting risk is very simple in concept but very complex in application. Essentially, all risk calculations use a similar method: a prior risk estimate is taken and using Bayes theorem, the influences of risk factors are added to derive a more accurate posterior risk estimate. This is not as simple as it seems because any prediction algorithm works best in the population it was derived from. Thus, the Framingham Heart Study data, which was derived from a US Caucasian population, significantly over-estimates risk in Asian populations,7 as seen in a study comparing the Framingham Risk Score, SCORE (Systematic Coronary Risk Evaluation) and the WHO/ISH (World Health Organization/International Society of Hypertension) prediction models.8
|
The most important thing to remember is that the correct risk scoring system must be used for the population being screened. |
Risk calculation algorithms
There are a very large number of CVD risk calculation algorithms available. Only a few are now relevant as many have become obsolete because they were either based on small data sets or on narrow populations. Currently useful risk scoring algorithms include:
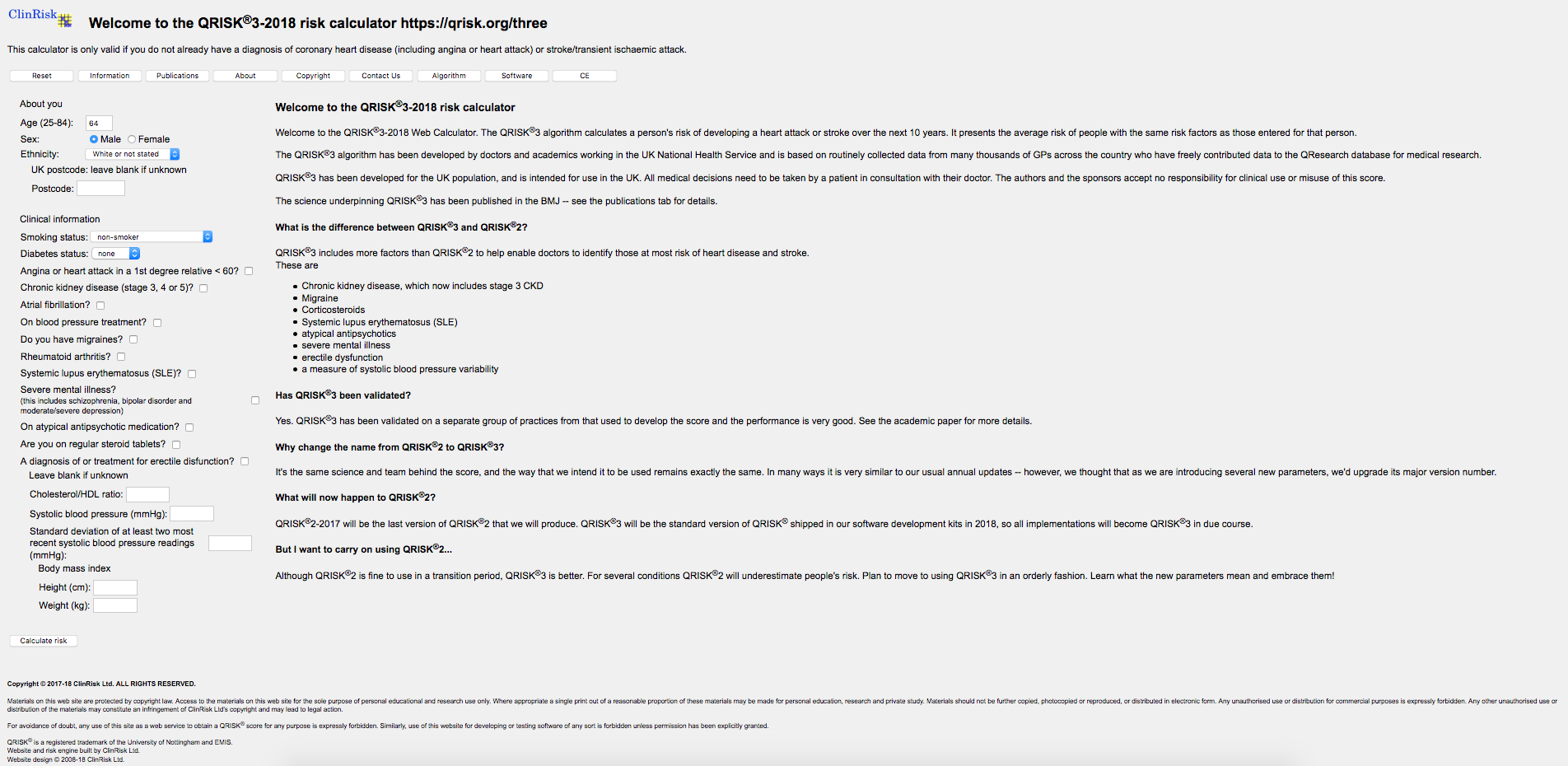
- QRISK®3 (Cardiovascular Risk Score), the latest iteration of a calculator developed by doctors and academics working in the UK National Health Service based on routinely collected data from many thousands of general practitioners (GPs) across the country who have freely contributed data to the QResearch database for medical research (figure 1, https://qrisk.org/)
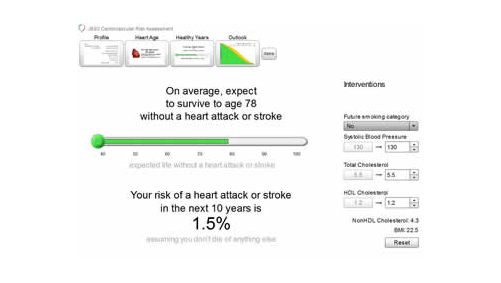
- JBS3 (Joint British Society for the Prevention of Cardiovascular Disease) calculator, derived from the recommendations of the JBS3 report9 (figure 2, http://www.jbs3risk.com/pages/risk_calculator.htm)
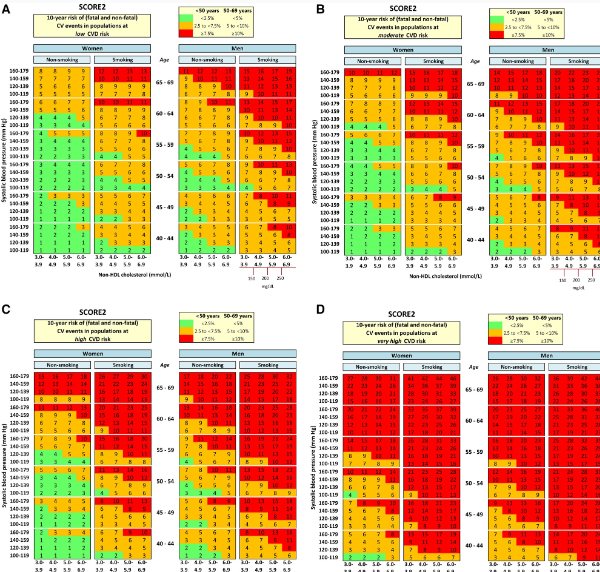
- SCORE2 risk calculator, previously SCORE, published by the European Society of Cardiology and derived from population studies in Europe. It provides risk calculations calibrated by country (figure 3, https://www.heartscore.org/en_GB)
How accurate are risk calculation algorithms?
An algorithm is only as good as the data it is based on. Thus, Framingham-based algorithms are good at identifying people who look like Framingham residents; a lipid clinic-based screening algorithm is good at identifying lipid clinic patients; and a hypertension clinic-based screening algorithm is good at identifying hypertension clinic patients.10
It is already well known that within an individual there is considerable variability in lipid and blood pressure results. This means that there is also considerable variability in the cardiac risk estimates that are generated by the risk algorithm.11 Therefore, it is advisable to use the average of several results to estimate risk, rather than rely on a single point estimate.
Due to the variability of risk factor algorithm results, it is sensible to use a minimum number of options. GP computer systems in the UK usually include a QRISK®3 calculator. Many secondary care doctors will use a JBS3 algorithm as this is available as a mobile phone app. If those people using the risk calculators understand the limitations and use some common sense in their interpretation, these limitations are not too extreme.
Important limitations
As mentioned earlier, an important limitation of all algorithms is that they are only as good as the data they are fed. It is common practice that missing data is replaced by ‘interpolation’ of an ‘average’ value that a patient of similar characteristics would have (e.g. using 1.1 mmol/L as a substitute for a missing high-density lipoprotein [HDL] cholesterol result). This will generate a reasonable average risk estimate for large groups but for a given individual this may be an incorrect risk estimate. It is good practice to always attempt to obtain the missing information rather than to guess what it might be.
The National Institute for Health and Care Excellence (NICE) recommends in their clinical guideline on cardiovascular risk assessment and reduction (NG238)12 that standard CVD risk scores will underestimate risk in people who have additional risk because of underlying medical conditions or treatments. These groups include those:
- treated for HIV
- already taking medicines to treat CVD risk factors
- with serious mental health problems
- taking medicines that can cause dyslipidaemia, such as antipsychotic medication, corticosteroids or immunosuppressant drugs
- with autoimmune disorders such as systemic lupus erythematosus, and other systemic inflammatory disorders
- who have recently stopped smoking
- with hypertriglyceridaemia (>4.5 mmol/L).
Targeting risk modification strategies
Targeting of medical strategies based on risk estimates is common in clinical practice. For example, in obstetrics, calculating the risk of Down’s syndrome can be used to identify which women would benefit from being offered a diagnostic amniocentesis. People over 60 years old are offered a faecal immunochemical test to identify those who would benefit from a colonoscopy to check for bowel cancer. Thus, cardiovascular prevention is similar in using a risk strategy to identify those who may benefit but different because being above the risk threshold leads directly to an offer of treatment, rather than leading to a diagnostic test that identifies whether treatment is necessary.
Also, for CVD prevention, there are two elements of risk modification. Firstly, certain strategies are applied to all patients regardless of their risk: advice to quit smoking, to avoid obesity, to exercise, to only drink moderate quantities of alcohol, and to eat a healthy balanced diet that includes poly- and mono-unsaturated fats in preference to saturated fat.
Secondly, pharmaceutical strategies are reserved for those patients who will benefit the most. This is due to the need for there to be a cost-benefit from using drug treatment, and because there is also a risk due to the drugs being given. Thus, the use of cardiac risk assessment is important because it allows sensible rationing of resources to those who are most in need and who will most likely benefit. However, some categories of patients require risk reduction treatment regardless of their risk, whilst others only need them if their risk exceeds the critical threshold. The groups whose baseline characteristics push them above the critical risk threshold where drug treatment is considered beneficial include patients with:
- established CVD
- diabetes mellitus (DM)
- established hypertension (blood pressure >160/100 mmHg), and end-organ damage
- chronic kidney disease (CKD)
- familial hypercholesterolaemia (FH)
- age >85 years (because their risk exceeds the risk threshold simply because of age)
- severe obesity (body mass index [BMI] >40 kg/m2).
|
The 2023/24 National Health Service (NHS) England Quality and Outcomes Framework (QOF) CHOL002 indicator recommends that patients on the QOF Coronary Heart Disease, Peripheral Arterial Disease, or Stroke/Transient Ischaemic Attack (TIA) Register should have a recording of non-HDL cholesterol <2.5 mmol/L, or where unavailable, a recording of LDL cholesterol <1.8 mmol/L in the preceeding 12 months.13 For more information, please watch this short video: https://tv.bjcardio.co.uk/cardiovascular-medicine/qof-indicators-for-cvd-prevention/) |
Other groups of patients should not be routinely given drug therapy unless and until their risk exceeds the critical threshold, which is currently considered to be a 10-year CVD risk of 10%.
Who should we screen?
In England and Wales, the prime source of information for policy is NICE (www.nice.org.uk). In Scotland, the Scottish Intercollegiate Guideline Network (SIGN) (www.sign.ac.uk) is the equivalent of NICE, and in Northern Ireland there is no formal equivalent to NICE but NICE policies are generally accepted as policy. This is then applied within the NHS screening programs to ensure all of the population is given optimum care at the right time.
In its 2023 Clinical Knowledge Summaries on CVD risk assessment and management,14 NICE recommends the following policy:
- Do not use opportunistic assessment as the main strategy in primary care to identify CVD risk in unselected people
- For the primary prevention of CVD in primary care:
- use a systematic strategy to identify people who are likely to be at high risk
- prioritise people on the basis of an estimate of their CVD risk before a full formal risk assessment — estimate their CVD risk using CVD risk factors already recorded in primary care electronic medical records
- prioritise people for a full formal risk assessment if their estimated 10-year risk of CVD is 10% or more
- people aged over 40 years should have their estimate of CVD risk reviewed on an ongoing basis
In England, all people aged 40–74 years are offered an NHS health check every five years, which includes an assessment of CVD risk.
- Once prioritised for assessment, it is then recommended that the QRISK®3 calculator is used to carry out the assessment, using as complete an information set as possible, including:
- personal details — age, sex, ethnicity, postcode
- clinical information — smoking status, and selected medical and family history, systolic blood pressure and standard deviation of at least two most recent systolic blood pressure readings, height and weight, and the total cholesterol/HDL-cholesterol ratio from a non-fasting blood sample
- It is also suggested that for certain patients who are considered high risk (e.g. people with type 1 DM, patients with stages 3, 4 and 5 CKD), it may be valuable to calculate risk because this will help patients make an informed choice about lipid-lowering therapy.
What do we do with patients who are at low risk?
A low-risk result does not mean that the patient is immune to developing CVD – it simply means that their current risk does not reach the threshold where risk of treatment versus risk of no treatment and the cost-benefit are in favour of treatment. Reassessment is expected to be offered every five years, or when there are any significant changes in, or new information about, family history. NICE NG238 recommends the consideration of treatment with atorvastatin 20 mg for the primary prevention of CVD, if they have an informed preference for taking a statin or there is concern that risk may be underestimated.12 This may be particularly important in young people who have a significant risk factor e.g. hypercholesterolaemia or significant family history of premature CVD; their 10-year risk may be low, but their lifetime risk will be high.
|
The decision of whether to offer treatment in these cases will be on a case-by-case basis using shared decision-making. |
What do we do about patients who are borderline risk?
If a patient’s risk is below the threshold by a fraction (e.g. 9.8%), it is good practice to calculate what their risk would be in a couple of years. This allows discussion about whether the patient wants treatment to be initiated immediately, even though they are not quite at the risk threshold, or whether they would prefer to be reassessed earlier than the standard five years. Be aware that all CVD risk assessment tools can provide only an approximate value for CVD risk. Interpretation of CVD risk scores should always reflect informed clinical judgement.
|
NICE NG238 recommends that doctors consider atorvastatin 20 mg for the primary prevention of CVD for people with a 10-year risk of less than 10% where the person is happy to take a statin or there is concern that the person’s risk of a cardiovascular event may be underestimated.12 Here, a lifetime risk tool such as QRISK®3-lifetime can inform discussions on CVD risk. |
What do we do with patients who are at high risk?
Patients identified at high risk need to be assessed to determine whether lifestyle modification is appropriate and use of lipid-lowering therapy needs to be considered. This is covered in module 4 of this lipids programme.
Lipoprotein(a) is an additional risk factor
|
Lipoprotein(a) (Lp[a]) is an additional independent cardiovascular risk factor associated with atherosclerosis and calcified aortic valve stenosis.15,16 |
Levels are mainly determined by genetic factors with lifestyle having little or no influence. Lp(a) levels are high in African populations and lower in Chinese and Japanese populations. Patients with Lp(a) levels >120 nmol/L or >50 mg/dL have an increased risk of developing CVD. Lp(a) is not currently recommended for risk screening in the general population. The European Atherosclerosis Society recommends measuring Lp(a) at least once in a person’s lifetime to identify those adults at high risk of CVD with a premature history of CVD, family history of atherosclerosis, family history of high levels of Lp(a), and FH.16
The Lp(a) risk calculator is a useful tool to estimate CVD risk in patients with elevated Lp(a) levels; it highlights how the CVD risk can be significantly underestimated when elevated Lp(a) levels are not considered in estimating the CVD risk. While specific treatments are currently unavailable to lower Lp(a), this tool gives importance to managing the modifiable risk factors.
The Lp(a) risk calculator is available at: https://www.lpaclinicalguidance.com/
Further information sources
The incidence of CVD varies depending on local factors. The government publishes standard information packs tailored for every clinical commissioning group across the country so that the importance of CVD as a local risk factor can be reviewed.17
Key learning messages
- All screening programmes are designed to ensure that there is a favourable balance between benefit and harm, and that the benefit is cost effective
- A number of ‘risk engines’ have been validated but QRISK®3 is the choice with which to assess CVD risk for primary prevention
- Screening programs are appropriate for primary prevention (where there is no evidence of prior disease)
- The risk threshold for the consideration of statin therapy for primary prevention is now 10% or greater 10-year risk of developing CVD
- Screening is not appropriate for secondary prevention (where there is evidence of disease) – in these patients, treatment is appropriate
- Screening is not appropriate for patients with CKD, DM or FH – these conditions are considered to be equivalent to a CVD event and should be treated as if they require secondary prevention
- QRISK®3 can be used to demonstrate risk levels to patients with CKD or type 1 DM to help them understand why treatment is a good idea.
close window and return to take test
References
- British Heart Foundation. Heart statistics. 2024. Available at https://www.bhf.org.uk/-/media/files/for-professionals/research/heart-statistics/bhf-cvd-statistics-uk-factsheet.pdf (last accessed 21 March 2024)
- The Framingham Heart Study. Three generations of research on heart disease. Available at https://framinghamheartstudy.org (accessed 21 January 2024)
- The Framingham Heart Study. FHS celebrating its 75th anniversary. Available at https://www.framinghamheartstudy.org/fhs-celebrating-its-75th-anniversary/ (accessed 21 March 2024)
- Yusuf S, Hawken S, Ounpuu S et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52. http://dx.doi.org/10.1016/S0140-6736%2804%2917018-9
- Morris JN, Heady JA, Raffle PA, Roberts CG, Parks JW. Coronary heart-disease and physical activity of work. Lancet 1953;265:1053–7. https://doi.org/10.1016/S0140-6736(53)90665-5
- Ferrie JE, Shipley MJ, Davey Smith G, Stansfeld SA, Marmot MG. Change in health inequalities among British civil servants: the Whitehall II study. J Epidemiol Community Health 2002;56:922–6. http://dx.doi.org/10.1136/jech.56.12.922
- Asia Pacific Cohort Studies Collaboration. Cardiovascular risk prediction tools for populations in Asia. J Epidemiol Community Health 2007;61:115–21. http://dx.doi.org/10.1136/jech.2005.044842
- Selvarajah S, Kaur G, Haniff J et al. Comparison of the Framingham Risk Score, SCORE and WHO/ISH cardiovascular risk prediction models in an Asian population. Int J Cardiol 2014;176:211–8. https://doi.org/10.1016/j.ijcard.2014.07.066
- JBS3 Board. Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3). Heart 2014;100:678–9. http://dx.doi.org/10.1136/heartjnl-2014-305693
- Reynolds TM, Twomey PJ, Wierzbicki AS. Concordance evaluation of coronary risk scores: implications for cardiovascular risk screening. J Curr Med Res Opinion 2004;20:811–8. https://doi.org/10.1185/030079904125003647
- Reynolds TM, Twomey PJ, Wierzbicki AS. Accuracy of cardiovascular risk estimation for primary prevention in patients without diabetes. J Cardiovasc Risk 2002;9:183–90. https://doi.org/10.1177/174182670200900402
- National Institute for Health and Care Excellence (NICE). Cardiovascular disease: risk assessment and reduction, including lipid modification. Clinical guideline [NG238]. London: NICE, 2023. Available at https://www.nice.org.uk/guidance/ng238 (accessed 21 January 2024)
- NHS England. Quality and Outcomes Framework Guidance for 2023/24. 2023. Available at: https://www.england.nhs.uk/long-read/quality-and-outcomes-framework-guidance-for-2023-24/ (accessed 25 March 2024)
- National Institute for Health and Care Excellence (NICE). Clinical Knowledge Summaries: CVD risk assessment and management. Scenario: assessing cardiovascular risk. London: NICE, 2023. Available at https://cks.nice.org.uk/topics/cvd-risk-assessment-management/management/cvd-risk-assessment/ (accessed 21 January 2024)
- Mach F, Baigent C, Catapano AL et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41:111–88. https://doi.org/10.1093/eurheartj/ehz455
- Cegla J, Neely RDG, France M et al. HEART UK consensus statement on lipoprotein(a): a call to action. Atherosclerosis 2019;291:62–70. https://doi.org/10.1016/j.atherosclerosis.2019.10.011
- Public Health England. Cardiovascular disease profiles: May 2020 update. Available at https://www.gov.uk/government/statistics/cardiovascular-disease-profiles-may-2020-update (accessed 21st January 2024)

All rights reserved. No part of this programme may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the publishers, Medinews (Cardiology) Limited.
It shall not, by way of trade or otherwise, be lent, re-sold, hired or otherwise circulated without the publisher’s prior consent.
Medical knowledge is constantly changing. As new information becomes available, changes in treatment, procedures, equipment and the use of drugs becomes necessary. The editors/authors/contributors and the publishers have taken care to ensure that the information given in this text is accurate and up to date. Readers are strongly advised to confirm that the information, especially with regard to drug usage, complies with the latest legislation and standards of practice.
Healthcare professionals should consult up-to-date Prescribing Information and the full Summary of Product Characteristics available from the manufacturers before prescribing any product. Medinews (Cardiology) Limited cannot accept responsibility for any errors in prescribing which may occur.