In a retrospective, case-controlled study, we examined the influence of diagnostic cardiac catheterisation (DCC) on the management of a cohort of very elderly patients (aged over 80 years). Peri-procedure complications were also determined. Study and control patients (aged less than 70 years) were randomly selected from patients who had undergone DCC over the previous five years. Data were collected on the primary treatment outcome (immediately following DCC) and the secondary outcome – the treatment the patient eventually received. We found that, while those in the very elderly group (n=100) were more likely to be referred for surgical intervention as a primary outcome, there was no overall difference in secondary outcome between the two groups. There was no difference in peri-procedural complications between the two groups. We observed that, in very elderly patients, DCC is both safe and contributes to clinical management to a similar degree compared with younger patients.
Introduction
Little observational data exist on the outcome of diagnostic cardiac catheterisation (DCC) in older people. In England and Wales, the population aged over 80 years is growing faster than any other age group.1DCC in these older patients may reveal widespread and complex coronary disease less suitable for percutaneous coronary intervention (PCI), and age-related comorbidity may preclude surgical intervention.
We conducted a retrospective, case-controlled study to examine the outcome, influence on management and complications of DCC in patients aged 80 years and older. The findings were compared with patients aged less than 70 years who had DCC over the same period.
Method
A total of 17,325 patients underwent DCC at the Silver Heart Unit, a secondary referral centre within a district general hospital between January 2005 and November 2010. We used computer-generated random numbers to identify 100 patients aged 80 years and older at the time of DCC (group A). A control group (group B) of 100 patients under 70 years of age at the time of DCC was identified by the same method. All patients had been referred for assessment of suspected coronary artery disease (CAD). Patients referred for DCC for other reasons (e.g. valvular heart disease) were not included. Clinical and demographic information was obtained from clinic letters and the computerised pathology system. For each patient the following data were obtained:
- Age and gender
- Elective or emergency procedure
- Number of angina medications at the time of DCC
- Cardiovascular risk factors:
- total cholesterol (>5 mmol/L)
- diabetes
- renal impairment (estimated glomerular filtration rate [eGFR] <60 ml/min)
- hypertension
- smoking status
- peripheral vascular disease (PVD)
- history of transient ischaemic attack (TIA) or stroke.
The ‘primary outcome’ was the preferred intervention following DCC, and the ‘secondary outcome’ was the intervention the patient eventually received. Both decisions were documented, as were any complications relating to the DCC.
Data were collected from online systems and verified by comparing the data with the hospital case notes in a small, randomly selected sample of 10 patients in each group.
Data were analysed using the Chi-squared statistic and Student’s unpaired t-test.
Results
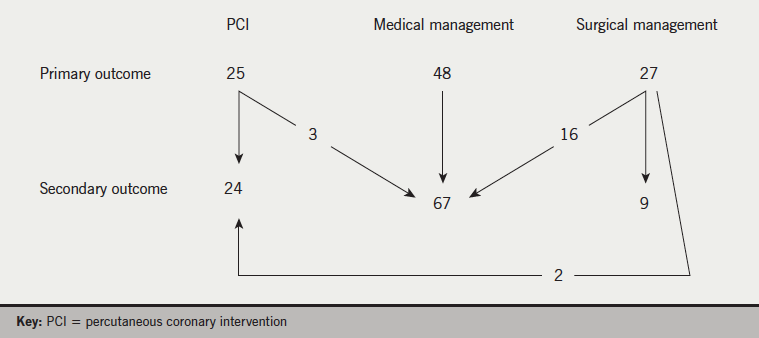
Between January 2005 and November 2010, 17,325 patients underwent DCC, of whom 771 (4%) were aged 80 or over.The characteristics of the two groups of patients are presented in table 1. Primary and secondary outcomes following DCC are presented in table 2 and figures 1 and 2.

More patients from group A were referred for surgery compared with group B (p<0.001). From the 27 patients in group A referred for surgery, 13 were considered unfit for surgery (on the grounds of comorbidity) and a further five patients declined surgery. Only one patient in group B referred for surgery (primary outcome), did not receive surgery. Overall, there was no difference in the final revascularisation rates between the two groups of patients. Of the 18 patients in group A who did not receive surgery (primary outcome), nine were dead within 3.5 years. The corresponding mortality for the entire elderly cohort was 25 (p<0.01).
There were no significant differences in complication rates following DCC between the two patient groups (table 3).

Discussion
In older patients we observed that DCC is safe, and contributes to clinical management in a similar way to that seen in younger patients.
Following DCC, 52% of our older group were referred for revascularisation as the ‘primary outcome’ compared with 40% of younger patients. These findings are similar to previous reports of revascularisation rates in older cohorts: Thompson et al.2 reported that, in patients aged over 75 years of age, 31% and 28% of Canadian men were referred for bypass surgery (CABG) and PCI, respectively. The corresponding values for older Canadian women were 18% and 29%, and the overall referral rates for revascularisation were comparable with a younger cohort. Niebauer et al.3 reported referral rates of 31% and 35%, respectively, for CABG and PCI from 1,085 consecutive patients aged over 80 years.
Primary treatment decision was generally determined by an interventional cardiologist and patient. Secondary outcome was generally determined by the interventional cardiologist and surgeon in the context of an informal multi-disciplinary team (MDT).
Before the widespread introduction of PCI, Elder et al.4 compared ‘primary’ and ‘secondary’ outcomes from DCC in patients aged over 70 years with suspected CAD. The findings were compared with patients aged under 70 years. Referral rates (‘primary outcome’) for revascularisation (predominantly CABG) were 48% and 42% for the older and younger cohorts, respectively.
We made a distinction between the ‘primary outcome’, based on the management plan immediately following DCC, and the treatment actually received, which we termed ‘secondary outcome’. Thus, ‘primary outcome’ would, in most instances, be determined by the cardiologist performing the DCC and would be heavily influenced by the coronary anatomy itself. The ‘primary outcome’ would often be recorded before consultation with the patient and without detailed knowledge of comorbidity, or patient preference. Perhaps, most importantly, the ‘primary outcome’ would be recorded before formal consultation with surgical colleagues, perhaps explaining why a significant proportion of these patients were subsequently considered unsuitable for CABG. Despite these considerations, we found that a similar proportion of patients from each age group ultimately underwent revascularisation. Compared with the older age group, almost all patients from the younger age group received the allocated ‘primary outcome’ decision, whether this was revascularisation or medical therapy.
In Elder’s study,4 the majority of patients (246 from 268) received the ‘primary outcome’ decision; thus, in the older cohort, only four patients from the 57 referred for CABG (primary outcome) did not eventually undergo surgery. In our older cohort, only six from 27 patients referred for surgery received the ‘primary outcome’ decision, perhaps reflecting both the advanced age of our patient cohort and the availability of less invasive revascularisation options; two patients who were considered unfit for surgery subsequently received PCI.
We observed that half of our older patients who did not receive surgery (as ‘primary outcome’) were dead within three years. Thompson et al.2 reported that the outcome of patients who did not undergo proposed surgery (as ‘primary outcome’) was poor, and considerably worse when compared with those patients who did receive either PCI or medical therapy as their ‘primary outcome’. Being considered unfit for surgery often reflects significant comorbidity, with advanced CAD, and ultimately a poor prognosis.5
Our older group were taking significantly more angina medications, had more documented cardiovascular risk factors, and presented more often as an emergency compared with the younger patient group. The older patients were also found to have more advanced CAD, and significantly more were referred for revascularisation. These findings are not unexpected given the predominant influence of age on cardiovascular risk profile and the natural history of CAD.
Complications rates associated with DCC were similar in both patient groups, with no strokes or deaths in the older patient group, and were consistent with previous studies.3
We agree that increasing the numbers would increase the overall strength of the study. However, in the context of an observational study, we feel that the relative group numbers (100 from 771 patients overall) were representative and that increasing group sizes would not materially affect the outcome.
Acknowledgement
The authors wish to thank Mr Sam Hampson for his kind help editing this paper.
Conflict of interest
None declared.
Editors’ note
See also the editorial in this issue by Green et al (doi: 10.5837/bjc.2014.001) on pages 7–8 of this issue.
Key messages
- Very elderly patients (aged over 80) are more likely to be referred for consideration of surgical intervention following diagnostic cardiac catheterisation (DCC)
- There is no difference in treatment outcome (percutaneous intervention or surgical intervention) between patients aged over 80 years compared with those under 70 years, irrespective of referral decision from DCC
- We found no difference in peri-procedural complications between patients aged under 70 and those aged over 80 years
References
1. Office for National Statistics. Mid-year population estimates. June 2011. Available from: http://www.statistics.gov.uk/cci/nugget.asp?id=949
2. Thompson CR, Humphries KH, Gao M et al. Revascularization use and outcomes after cardiac catheterization in British Columbia and Alberta. Can J Cardiol 2004;20:1417–23.
3. Niebauer J, Sixt S, Zhang F et al. Contemporary outcome of cardiac catheterizations in 1085 consecutive octogenarians. Int J Cardiol 2004;93:225–30. http://dx.doi.org/10.1016/S0167-5273(03)00216-X
4. Elder AT, Shaw TDR, Turnbull CM et al. Elderly and younger patients selected to undergo coronary angiography. BMJ 1991;303:950–3. http://dx.doi.org/10.1136/bmj.303.6808.950
5. Hemingway H, Crook AM, Feder G et al. Underuse of coronary revascularization procedures in patients considered appropriate for revascularization. N Engl J Med 2001;344:645–54. http://dx.doi.org/10.1056/NEJM200103013440906


