A. Menarini Farmaceutica Internazionale SRL has provided an educational grant for the production of this e-learning programme and has had no editorial control or input. The views and content expressed within this programme are solely those of the authors.
PP-CA-UK-0149 Date of preparation: March 2020
Atherosclerosis is an insidious process that develops over decades before presentation.1 Furthermore, first presentation can be a fatal event and those with symptomatic angina often have advanced underlying disease. The major risk factors for atherosclerosis are well defined2 and there is undeniable evidence that modification reduces risk. Therefore prevention is a cornerstone in the management of populations and individuals with or at risk of cardiovascular disease (CVD).
Two contrasting, but complimentary approaches, apply to CVD prevention.3 A high-risk strategy targets individuals with unfavourable risk factor profile. This can manifest as prescription of preventive medications or enrolment in structured lifestyle programmes. A population-based approach aims to modify CVD risk through lifestyle and environmental changes such as smoking bans or sugar taxes.
CVD risk screening
Screening for CVD, alongside stroke, diabetes, kidney disease, and dementia has been implemented in the UK since 2012. Adults aged 40–74 without a diagnosis of the above are invited to their primary care trust for a health check every five years. During the consultation, an individual’s risk is assessed, communicated, and managed.
Between April 2013 and March 2018, 4.9 million individuals had the health check from an eligible population of 15 million. Since 2009 the take up rate has improved to 48.4%, albeit it is some way off the 75% target set by the Department of Health. There are concerns about the overall benefit of the programme4 and limited evidence of its effectiveness.5,6 It is legally mandated, supported politically, and well received by patients, however, so it is likely to continue.
CVD risk prediction
The concept of total CVD risk estimation is essential in the prevention of CVD so as to treat individuals as a whole, rather than a selection of individual isolated risk factors. Total CVD risk also helps to takes into account that risk factors interact. For example, a 5 kg weight loss is associated with a 5 mmHg decrease in systolic blood pressure.7 Multiple validated CVD risk prediction calculators have been developed to predict an individual’s CVD risk. The majority are only suitable for those without any evidence of CVD except the SMART risk score specifically designed for predicting recurrent events in a secondary prevention population.
CVD risk prediction models utilise cohorts of individuals with recorded risk factors and CVD events to model the relative impact of each risk factor on the chances of manifest CVD. Typical risk factors included are: age, sex, ethnicity, family history, smoking status, body mass index (BMI), blood pressure, cholesterol (total and high-density lipoprotein).
The current standard8 risk prediction model in England and Wales is the QRISK39 model developed by Professor Julia Hippisley-Cox (University of Oxford) and a team at Nottingham University who developed previous models10,11 that have been validated within the UK population.12,13 The QRISK3 model (see figure 1) expands on traditional CVD risk factors to include: chronic kidney disease, atrial fibrillation, migraines, rheumatoid arthritis, systemic lupus erythematous, severe mental illness, atypical antipsychotic medication, regular steroid therapy, and erectile dysfunction.
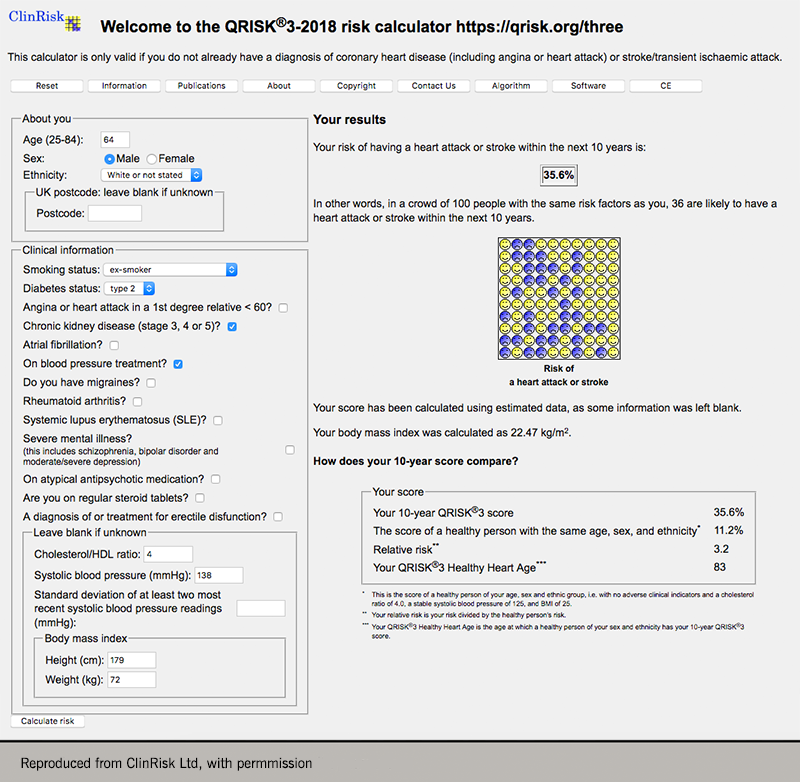
QRISK®3 provides multiple outputs in order to communicate an individual’s risk. The traditional absolute 10-year risk of a CVD event determines whether to recommend a trial of lifestyle modification and, if this is ineffective or inappropriate, pharmacological therapy targeted at lipid profile and blood pressure.8 The current threshold in the UK is an estimated risk of 10% or more having previously been 20% in 2014.14 There is much debate on the absolute threshold to trigger intervention bought about the by the change in 2014 and the merits of such a prescriptive threshold. Current American guidelines15 advocate a lower 7.5% threshold. The level of risk for intervention is not absolute but is a product of resources and health economics.
To counter the issues surrounding 10-year absolute risk since the publication of the Joint British Societies Guidelines on the Prevention of Cardiovascular Disease (JBS3)16 in 2014, there has been an equal emphasis on lifetime CVD risk. Lifetime risk is calculated by estimating the age of someone of the same gender and ethnicity, and same annual risk of an event, but with all the other risk factors at ‘optimal levels’. This is presented in the form an individual’s ‘heart age’ (see figure 2). This is easily understood and can lead to an improved risk factor profile at one year compared to presenting absolute risk alone.17 It has been integrated into multiple models worldwide.
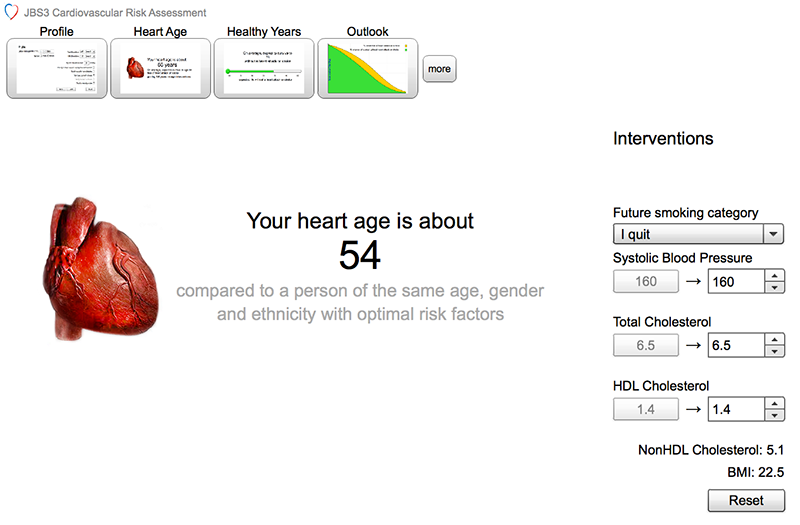
A lifetime approach targets the young as a significant determinant of CVD prediction models is age and we know that the atherosclerotic process precedes this by many decades. Therefore there is opportunity to assess and intervene early to modify the disease process. It also targets women who have a high lifetime risk that isn’t as recognised by 10-year estimation alone.
NHS Scotland advocates the use of the ASSIGN score,18,19 which was developed from random prospective cohort studies within Scottish populations. The European Society of Cardiology (ESC) recommends SCORE (Systemic Coronary Risk Estimation), which is developed in a similar manner as the ASSIGN score using pan-European populations.20 These contrast to the QRISK family that are built upon data routinely collected from English and Welsh general practitioners surgeries. QRISK®3 has excellent performance for UK populations compared to other available models.9
CVD risk factors
An individual’s total CVD risk is a combination of numerous modifiable and non-modifiable risk factors (table 1). As seen earlier, these risk factors don’t act in isolation but interact and multiply their CVD impact. The use of a validated CVD risk model is essential to guide the intensity of treatment.
Table 1. Risk factors used in estimating an individual’s risk of cardiovascular disease
| Non-modifiable | Modifiable | Emerging |
|---|---|---|
| Age | Cigarette smoking | Connective tissue disease |
| Gender | Dyslipidaemia | Migraine |
| Family history | Hypertension | Severe mental illness |
| Ethnicity | Diabetes mellitus | Obstructive sleep apnoea |
| Obesity and abdominal adiposity | ||
| Atherogenic diet | ||
| Physical inactivity and low fitness | ||
| Excess alcohol intake |
Cigarette smoking
Cigarette smoking is a major cause of CVD and is the single most preventable cause of death worldwide.21 Acute cigarette inhalation induces increased myocardial oxygen demand, increased heart rate, and blood pressure. Chronic inhalation leads to endothelial dysfunction, decreased high-density lipoprotein (HDL), and a systemic inflammatory response.22
Public health interventions have been a great success and current smoking prevalence in the UK is at an all-time low of 14.4%.23 Prevalence is not equally spread; smoking remains highest among the unemployed and manual workers.
Cigarette smoking triples the risk of non-fatal myocardial infarction compared to never smoking,24 there are also similar increases in the risk of sudden cardiac death.22 Cessation of cigarette smoking is a priority as it brings about a cost-effective25 rapid decline in the risk of future CVD events. In those with CVD there is a 50% reduction in premature death and 36% reduction in non-fatal future events.26
Of note, an individual would have to gain 16 units in body mass index (BMI) to offset the harmful effects of smoking.27
E-cigarettes (EC)
The rapid uptake of EC worldwide and in the UK has been a challenge to health professionals wanting to provide individuals with robust evidenced based advice. Current estimates for prevalence in the UK for all adults is 5.4–6.2% and 14.9–18.5% of smokers.28
A review29 on the acute effects of EC on the cardiovascular system reports measurable detrimental effects on heart rate, blood pressure, and oxidative stress. These effects, however, were not consistent in all reviewed studies and when compared to cigarette smoking appeared to be to a lesser extent. There is emerging evidence that use of ECs is associated with an increased risk of myocardial infarction.30,31
Current NICE guidance32 states that, “e-cigarettes are substantially less harmful… but are not risk free”. For example, there have been anecdotal reports from the US in 2019 of deaths that may be associated with e-cigarette use.
Dyslipidaemia
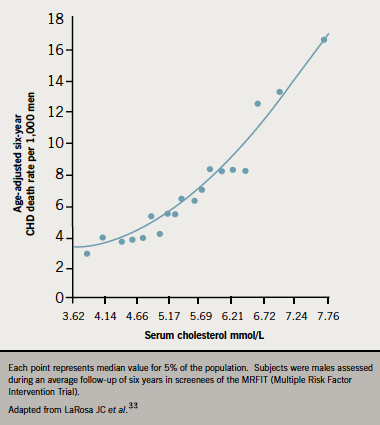
There is undeniable evidence that dyslipidaemia, especially elevated serum cholesterol, is a major risk factor for the development of CVD (figure 3).33,34 There are numerous measurable lipid parameters, the most commonly used are: total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein (HDL-C), non-HDL-C (a combination of various atherogenic lipoproteins including LDL-C). TC and HDL-C are essential components of QRISK3,9 SCORE,20 and ASSIGN19 models.
Treatment of dyslipidaemia is targeted at the reduction of LDL-C, typically with statins, as this has proven to reduce the risk of CVD.35 Those with the highest level derive the greatest benefit but all individuals benefit regardless of risk.36,37 A 1 mmol/L LDL-C reduction is associated with a 22% risk of a CVD event.35
Hypertension
Hypertension is defined as an office blood pressure (BP) >140/90 mmHg38,39 or >135/85 mmHg using ambulatory blood pressure monitoring. Worldwide 47% of ischaemic heart disease and 13.5% of premature deaths can be attributed to hypertension. Hypertension affects one in four adults in England and was responsible for 75,000 deaths in 2015.40,41
The relationship between angina and hypertension has been proven since the 1960s.42 Meta-analyses consistently shows benefit in treatment in all-cause and CVD mortality.43–45 The current blood pressure target in the UK is <140/90 mmHg in those under 80 and <150/90 mmHg in those above.
There is a growing body of evidence that a more intensive approach to a lower target blood pressure can be of benefit to prevent CVD events. The SPRINT trial,46 comparing a SBP target of 120 mmHg versus 140 mmHg, showed a 25% reduction in CVD events in the more intensive group. This finding has not been consistently replicated. A Cochrane review47 of standard target (<140–160/90–100 mmHg) versus intensive target (<135/85 mmHg) found no difference in CVD mortality.
Diet
In 2017, 11 million deaths worldwide were attributed to poor diet.48 Numerous individual dietary components have all been studied in their relation to the development of CVD. The vast array of macro and micro dietary components and their individual effect on CV risk is too wide to explore in detail here.
Stepping back from individual components of food and assessing intake as a whole has led to the promotion of cardioprotective diets. The best known of these is the Mediterranean diet developed from the dietary habits of the Mediterranean basin from the 1960s.49 It is high in fruits, vegetables, legumes, complex carbohydrates and fish alongside olive oil as the main source of fat.
The Mediterranean diet has been itemised into a 14–point score49 (table 2) and is used as part of the cardiac rehabilitation programme in the NHS. Increasing two points on the score is 10% reduction in CV mortality and -8% in overall mortality.50 There are also measurable reductions in cancer and neuro-degenerative diseases.
Table 2. Validated 14-item questionnaire of Mediterranean diet adherence
| Questions | Criteria for 1 point |
|---|---|
| Do you use olive oil as main culinary fat? | Yes |
| How much olive oil do you consume in a given day (including oil used for frying, salads, out-of-house meals, etc.)? | ≥4 table spoons |
| How many vegetable servings do you consume per day? (1 serving: 200 g [consider side dishes as half a serving]) | ≥2 (≥1 portion raw or as a salad) |
| How many fruit units (including natural fruit juices) do you consume per day? | ≥3 |
| How many servings of red meat, hamburger, or meat products (ham, sausage, etc.) do you consume per day? (1 serving: 100–150 g) | <1 |
| How many servings of butter, margarine, or cream do you consume per day? (1 serving: 12 g) | <1 |
| How many sweet or carbonated beverages do you drink per day? | <1 |
| How much wine do you drink per week? | ≥7 glasses |
| How many servings of legumes do you consume per week? (1 serving: 150 g) | ≥3 |
| How many servings of fish or shellfish do you consume per week? (1 serving: 100–150 g of fish or 4–5 units or 200 g of shellfish) | ≥3 |
| How many times per week do you consume commercial sweets or pastries (not homemade), such as cakes, cookies, biscuits, or custard? | <3 |
| How many servings of nuts (including peanuts) do you consume per week? (1 serving 30 g) | ≥3 |
| Do you preferentially consume chicken, turkey, or rabbit meat instead of veal, pork, hamburger, or sausage? | Yes |
| How many times per week do you consume vegetables, pasta, rice, or other dishes seasoned with sofrito (sauce made with tomato and onion, leek, or garlic and simmered with olive oil)? | ≥2 |
| Reproduced from Martínez-González MA et al.49 with permission | |
Alcohol
Currently 14 units of alcohol per week is the recommended maximum in the UK. This shouldn’t be binged but spread across the week with several drink-free days.51 There is a consistent J-shaped trend and risk of CVD.
Moderate drinkers are at the lowest risk when compared to non-drinkers and heavy drinkers. Those who have 1–2 drinks per day are at the lowest risk of coronary artery disease mortality alongside a 25% risk reduction in CVD mortality.52
Despite benefits on CVD, excess alcohol intake is a widespread public health issue with a fifth of people in the UK drinking to excess with 5,800 alcohol related deaths in 2017.52
Physical inactivity and low fitness
Since the London Transport workers study of 1953 there has been a clear link between physical inactivity and CVD.53 Bus conductors, compared to drivers, were noted to have a significantly reduced risk of CVD attributed to their activity while at work.
Increasing physical activity and fitness is a priority since it is responsible for as many deaths as smoking in the UK. Since the 1960s we are 20% less active.54 Current guidelines recommend either 150 minutes of moderate intensity or 75 minutes of vigorous activity spread across the week. Fifteen minutes of exercise per day can decrease all-cause mortality by 14%.55
A Cochrane review55 of exercise-based cardiac rehabilitation (CR) in adults with stable angina found no impact nil benefit for all-cause mortality, myocardial infarction or CVD hospital admissions, review suffered from a low-quality evidence base however. For those post-MI or revascularisation exercise-based CR reduces risk of re-admission but had no impact on all-cause mortality or repeat MI.55
Obesity and abdominal adiposity
The prevalence of obesity is increasing worldwide with 29% of the UK having a BMI >30.56 If current rates remain, life expectancy estimates may regress by five years by 2050.57 Elevated BMI in adolescence increases the risk of coronary artery disease (CAD) by up to five-times. This effect is not attenuated by weight loss in adulthood.58
The distribution of fat is also an important predictor of CVD. Those that deposit centrally in the abdomen are at increased risk of diabetes, inflammation, and adverse lipid profile that predisposes to CVD.59
There may be an obesity ‘paradox’ in individuals with CAD having improved survival compared to those with normal BMI. With a three-year follow-up after non-ST elevation myocardial infarction (NSTEMI), obese individuals had a mortality of 3.6% compared to 9.9% for normal BMI.60 The mechanism for this finding is unknown. The impact of weight loss is not conclusive with some studies detecting better outcomes but others nil benefit.61
Diabetes mellitus (DM) and impaired glucose metabolism
Currently 4.7 million people in the UK have DM and this is set to rise to 5.5 million by 203062 with similar trajectories worldwide. Symptoms of DM are non-specific and up to 50% of cases are undiagnosed.62 CVD is the main cause of death in those with DM – this is driven by macrovascular disease alongside other risk factors of hypertension and dyslipidaemia.63
Target driven multi-factorial management of DM can prevent macrovascular complications in DM. In the STENO 2 trial,63 there was an absolute reduction in CVD events of 29% in the intensive group. Overly intensive blood glucose targets, however, can be harmful as realised in the ACCORD trial.51
Rheumatoid arthritis (RA)
Rheumatoid arthritis confers a 48% increased relative risk of CVD compared to the general population and leads to an excess mortality.64 Chronic inflammation present in RA can enhance atherogenesis.
Systemic lupus erythematosus (SLE)
As in RA, individuals with SLE have an excess risk of CVD as high as 9–50 fold compared to the general population.65 This excess is not explained by the presence of traditional risk factors supporting inflammatory processes promoting atherogenesis.
Severe mental illness (SMI)
Individuals with SMI (schizophrenia, bipolar and major depressive disorder) have a 51% increased risk of CAD compared to the general population.66 This excess risk stems from both lifestyle/behavioural factors in the SMI cohort alongside possible common biological factors.67
Migraine
Migraine is common and sufferers have been noted to have a mild excess in CVD. A meta-analysis68 reports a 29% risk of angina and 33% risk of MI. Proposed mechanisms69 for this include: endothelial dysfunction, vasospasm, presence of traditional risk factors, and hypercoagulability. Those with aura have a higher risk.
Obstructive sleep apnoea (OSA)
Sleep is not a passive process. Hypoxia from OSA induces sympathetic activity that adversely effects the myocardium.70 There is an excess morbidity and mortality in those with CVD and OSA but treatment with continuous positive airway pressure (CPAP) in the largest trial to date71 has shown nil change in mortality in those with CVD.
Management of CVD risk factors
Management of CVD risk factors can drastically improve outcomes. Furthermore, interventions available tend to be low cost and achievable on a population-wide basis. There is commonality in the risk factors for multiple non-communicable diseases, therefore management could bring improvements to cancer, chronic lung disease and neurodegenerative disorders.
Prevention of CVD requires intervention at the population level to engineer a heart-healthy environment. Classically these have focussed on cigarettes with increased taxation, banning of advertising (1985, 2003) and restricting smoking in public places (2007). The government has set an ambitious target of being ‘smoke free’ by 2030 in England.72 These legislative tactics are being used to combat child obesity73 in the form of sugary drink taxes, sugar reduction and limiting promotions.
Enabling behaviour change without legislation/regulation can be done through two broad mechanisms.74 Firstly a method of providing information designed to alter beliefs and attitudes and motivate behaviour change. This mechanism has traditionally been used for health promotion despite only being modestly effective at best. This is partly because it requires active engagement and a higher degree of cognitive capacity.
The second method, known as ‘nudging’, requires little or no cognitive capacity or active engagement. This method has classically been used by retailers and advertisers to ‘nudge’ people to purchase sweets and chocolate at the checkout aisle, or placing discount alcohol at their shop forecourt. This can be swapped for a positive nudge by placing fruit or health items in these areas. Voluntary nudging undertaken by private industry is consistently less effective than legislation.74
Individual CVD risk management takes place in multiple different settings. Primary care physicians play an essential role in the successful implementation of prevention guidelines. They are the key person to identify, initiate and monitor risk reduction strategies and the gatekeeper for onward referral for specialist services. In the UK they are also responsible for facilitating the five-year health checks described previously.
Within the setting of an acute event, management is typically in the hospital environment. Prescription of prognostic medications for discharge significantly reduces mortality.75 Having a structured enrolment process for cardiac rehabilitation for discharged patients significantly improves enrolment.76 In the NHS, all patients discharged post-MI should be assessed within 10 days by the cardiac rehabilitation team.
Cardiac rehabilitation is an evidence-based, multifactorial intervention designed to decrease morbidity and mortality in CVD, particularly after MI. In the modern era the current approach appears to have no effect on mortality but reduces re-admission.77
Key messages
- Screening for CVD is essential as those first presenting may have fatal or advanced disease
- CVD risk prediction models can accurately identify those who will benefit most from intervention
- Most risk factors are modifiable and have evidence of benefit for the individual
- Preventing CVD is a global priority requiring coordinated efforts from governments, health care systems and professionals, individuals and private industry.
Further learning
Additional study of the preventive aspects of cardiovascular disease can be obtained from the University of Galway MSc in Preventive Cardiology. Taught modules address the development and practical aspects of the discipline including a PGDip option.
https://www.nuigalway.ie/courses/taught-postgraduate-courses/preventive-cardiology.html
The ESC Textbook of Preventive Cardiology is an invaluable resource for those wishing to explore this field further.
close window and return to take test
References
- Rose G. Incubation period of coronary heart disease. BMJ 1982;284:1600–1. https://doi.org/10.1136/bmj.284.6329.1600
- Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52. https://doi.org/10.1016/S0140-6736(04)17018-9
- Rose G. Sick individuals and sick populations. Int J Epidemiol 2001;30(3):427–32. https://doi.org/10.1093/ije/30.3.427
- Capewell S, McCartney M, Holland W. Invited debate: NHS Health Checks–a naked emperor? J Pub Health (Bangkok) 2015;37(2):187–92. https://doi.org/10.1093/pubmed/fdv063
- Chang KC-M, Soljak M, Lee JT, et al. Coverage of a national cardiovascular risk assessment and management programme (NHS Health Check): Retrospective database study. Prev Med 2015;78:1-8. https://doi.org/10.1016/j.ypmed.2015.05.022
- Mytton OT, Jackson C, Steinacher A, et al. The current and potential health benefits of the National Health Service Health Check cardiovascular disease prevention programme in England: A microsimulation study. PLoS Med 2018;15(3):e1002517. https://doi.org/10.1371/journal.pmed.1002517
- The Hypertension Prevention Trial: three-year effects of dietary changes on blood pressure. Hypertension Prevention Trial Research Group. Arch Intern Med 1990;150(1):153–62. http://www.ncbi.nlm.nih.gov/pubmed/2404477. Accessed July 4, 2019
- National Institute for Health and Care Excellence (NICE). CVD risk assessment and management. https://cks.nice.org.uk/cvd-risk-assessment-and-management#!scenario. Published 2019. Accessed July 4, 2019
- Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ 2017;357:j2099. https://doi.org/10.1136/bmj.j2099
- Hippisley-Cox J, Coupland C, Vinogradova Y, et al. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: Prospective open cohort study. BMJ 2007;335:136–41. https://doi.org/10.1136/bmj.39261.471806.55
- Hippisley-Cox J, Coupland C, Vinogradova Y, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008;336:1475 https://doi.org/10.1136/bmj.39609.449676.25
- Hippisley-Cox J, Coupland C, Brindle P. The performance of seven QPrediction risk scores in an independent external sample of patients from general practice: a validation study. BMJ Open 2014;4(8):e005809. https://doi.org/10.1136/bmjopen-2014-005809
- Pike MM, Decker PA, Larson NB, et al. Improvement in Cardiovascular Risk Prediction with Electronic Health Records. J Cardiovasc Transl Res 2016;9(3):214–22. https://doi.org/10.1007/s12265-016-9687-z
- England N. NICE publishes new draft guidelines on statins use. https://www.nhs.uk/news/medication/nice-publishes-new-draft-guidelines-on-statins-use/. Published 2014.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;139(25). https://doi.org/10.1161/CIR.0000000000000625
- Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3). Heart 2014;100(Suppl 2):ii1-ii67. https://doi.org/10.1136/heartjnl-2014-305693
- Lopez-Gonzalez AA, Aguilo A, Frontera M, et al. Effectiveness of the Heart Age tool for improving modifiable cardiovascular risk factors in a Southern European population: a randomized trial. Eur J Prev Cardiol 2015;22(3):389–96. https://doi.org/10.1177/2047487313518479
- Woodward M, Brindle P, Tunstall-Pedoe H, SIGN group on risk estimation. Adding social deprivation and family history to cardiovascular risk assessment: the ASSIGN score from the Scottish Heart Health Extended Cohort (SHHEC). Heart 2005;93(2):172–6. http://dx.doi.org/10.1136/hrt.2006.108167
- Scotland N. ASSIGN Score Priotising Prevention of Cardiovascular Disease. http://www.assign-score.com/. Published 2007. Accessed July 4, 2019
- Conroy R, Pyörälä K, Fitzgerald AP, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003;24(11):987–1003. https://doi.org/10.1016/S0195-668X(03)00114-3
- Health Effects | Tobacco Atlas. https://tobaccoatlas.org/topic/health-effects/. Accessed July 15, 2019.
- Centers for Disease Control and Prevention (US). How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the Surgeon General. US: National Center for Chronic Disease Prevention and Health Promotion, 2010. https://www.ncbi.nlm.nih.gov/books/NBK53017/pdf/Bookshelf_NBK53017.pdf
- Public Health England. Turning the tide on tobacco: smoking in England hits a new low – public health matters. https://publichealthmatters.blog.gov.uk/2018/07/03/turning-the-tide-on-tobacco-smoking-in-england-hits-a-new-low/. Published 2018. Accessed July 15, 2019
- Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52. https://doi.org/10.1016/S0140-6736(04)17018-9
- Owen L, Shearn P, Younger T, et al. National Institute for Health and Care Excellence (NICE): Matrix evidence – smoking cessation in secondary care: cost-effectiveness review. https://www.nice.org.uk/guidance/ph48/evidence/review-of-cost-effectiveness-pdf-430365277 (last accessed 15 July 2019)
- Critchley JA, Capewell S. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease. JAMA 2003;290(1):86–97. https://doi.org/10.1001/jama.290.1.86
- Diverse Populations Collaboration. Smoking, body weight, and CHD mortality in diverse populations. Prev Med 2004;38(6):834–40. https://doi.org/10.1016/j.ypmed.2003.12.022
- McNeill A, Brose LS, Calder R, et al. Public Health England – vaping in England: an evidence update February 2019. London. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/781748/Vaping_in_England_an_evidence_update_February_2019.pdf
- Qasim H, Karim ZA, Rivera JO, et al. Impact of electronic cigarettes on the cardiovascular system. J Am Heart Assoc 2017;6(9). https://doi.org/10.1161/JAHA.117.006353
- Alzahrani T, Pena I, Temesgen N, Glantz SA. Association between electronic cigarette use and myocardial infarction. Am J Prev Med 2018;55(4):455–61. https://doi.org/10.1016/j.amepre.2018.05.004
- Bhatta DN, Glantz SA. Electronic cigarette use and myocardial infarction among adults in the US population assessment of tobacco and health. J Am Heart Assoc 2019;8(12):e012317. https://doi.org/10.1161/JAHA.119.012317
- National Institute for Health and Care Excellence. Stop smoking interventions and services. NICE guideline [NG92]. https://www.nice.org.uk/guidance/ng92/chapter/Recommendations#advice-on-ecigarettes (last accessed 15 July 2019)
- LaRosa JC, Hunninghake D, Bush D, et al. The cholesterol facts. A summary of the evidence relating dietary fats, serum cholesterol, and coronary heart disease. A joint statement by the American Heart Association and the National Heart, Lung, and Blood Institute. The Task Force on Cholesterol Issues, American Heart Association. Circulation 1990;81(5):1721–33. https://doi.org/10.1161/01.CIR.81.5.1721
- Marmot M, Elliott P. Coronary heart disease epidemiology. Oxford: Oxford University Press, 2005. https://doi.org/10.1093/acprof:oso/9780198525738.001.0001
- Cholesterol Treatment Trialists’ (CTT) Collaborators, Baigent C, Blackwell L, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010;376:1670–81. https://doi.org/10.1016/S0140-6736(10)61350-5
- Cholesterol Treatment Trialists’ (CTT) Collaborators B, Mihaylova B, Emberson J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 2012;380:581–90. https://doi.org/10.1016/S0140-6736(12)60367-5
- Brugts JJ, Yetgin T, Hoeks SE, et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trials. BMJ 2009;338:b2376. https://doi.org/10.1136/bmj.b2376
- National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. Clinical guideline [CG127].https://www.nice.org.uk/guidance/CG127/chapter/1-Guidance#diagnosing-hypertension-2. (last accessed 15 July 2019)
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018;39(33):3021–104. https://doi.org/10.1093/eurheartj/ehy339
- Public Health England. Health matters: combating high blood pressure, 2017. https://www.gov.uk/government/publications/health-matters-combating-high-blood-pressure/health-matters-combating-high-blood-pressure (last accessed 28 July 2019)
- Forouzanfar MH, Alexander L, Anderson HR, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:2287–323. https://doi.org/10.1016/S0140-6736(15)00128-2
- Richardson PJ, Hill LS. Relationship between hypertension and angina pectoris. Br J Clin Pharmacol 1979;7(Suppl 2):249S–53S. https://doi.org/10.1111/j.1365-2125.1979.tb04697.x
- Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet 2016;387:435–43. https://doi.org/10.1016/S0140-6736(15)00805-3
- Bundy JD, Li C, Stuchlik P, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality. JAMA Cardiol 2017;2(7):775–81. https://doi.org/10.1001/jamacardio.2017.1421
- Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338:b1665. https://doi.org/10.1136/bmj.b1665
- Group TSR. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373(22):2103–16. https://doi.org/10.1056/NEJMoa1511939
- Saiz LC, Gorricho J, Garjón J, et al. Blood pressure targets for the treatment of people with hypertension and cardiovascular disease. Cochrane Database Syst Rev July 2018. https://doi.org/10.1002/14651858.CD010315.pub3
- GBD 2017 Diet Collaborators A, Sur PJ, Fay KA, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019;393:1958–72. https://doi.org/10.1016/S0140-6736(19)30041-8
- Martínez-González MA, García-Arellano A, Toledo E, et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: The PREDIMED trial. PLOS ONE 2012;7(8):e431342012 https://doi.org/10.1371/journal.pone.0043134
- Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr 2010;92(5):1189–96. https://doi.org/10.3945/ajcn.2010.29673
- The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358(24):2545–59. http://doi.org/10.1056/NEJMoa0802743
- Ronksley PE, Brien SE, Turner BJ. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671 https://doi.org/10.1136/bmj.d671
- Morris JN, Heady JA, Raffle PA, et al. Coronary heart disease and physical activity of work. Lancet 1953;262:1053–7. https://doi.org/10.1016/S0140-6736(53)90665-5
- Public Health England. Physical activity: applying all our health. Published 2019. https://www.gov.uk/government/publications/physical-activity-applying-all-our-health/physical-activity-applying-all-our-health (last accessed 12 August 2019)
- Long L, Anderson L, Dewhirst AM, et al. Exercise-based cardiac rehabilitation for adults with stable angina. Cochrane Database Syst Rev. 02 February 2018. https://doi.org/10.1002/14651858.CD012786.pub2
- NHS UK. Statistics on obesity, physical activity and diet, England, 2019. https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/statistics-on-obesity-physical-activity-and-diet-england-2019 (last accessed 16 August 2019)
- Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on US life expectancy. N Engl J Med 2009;361(23):2252–60. https://doi.org/10.1056/NEJMsa0900459
- Tirosh A, Shai I, Afek A, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med 2011;364(14):1315–25. https://doi.org/10.1056/NEJMoa1006992
- Després J-P. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012;126(10):1301–13. https://doi.org/10.1161/CIRCULATIONAHA.111.067264
- Buettner HJ, Mueller C, Gick M, et al. The impact of obesity on mortality in UA/non-ST-segment elevation myocardial infarction. Eur Heart J 2007;28(14):1694–701. https://doi.org/10.1093/eurheartj/ehm220
- Artham SM, Lavie CJ, Milani R V, Ventura HO. Obesity and hypertension, heart failure, and coronary heart disease-risk factor, paradox, and recommendations for weight loss. Ochsner J. 2009;9(3):124–32. http://www.ncbi.nlm.nih.gov/pubmed/21603427 (last accessed 16 August 2019)
- Diabetes UK. Number of people with diabetes reaches 4.7 million. https://www.diabetes.org.uk/about_us/news/new-stats-people-living-with-diabetes (last accessed 27 August 2019)
- American Diabetes Association. Cardiovascular disease and risk management: standards of medical care in diabetes—2018. Diabetes Care 2018;41(Suppl 1):S103–S123. https://doi.org/10.2337/dc19-S010
- Kaasenbrood L, Boekholdt SM, van der Graaf Y, et al. Distribution of estimated 10-Year risk of recurrent vascular events and residual risk in a secondary prevention population. Circulation 2016;134(19):1419–29. https://doi.org/10.1161/CIRCULATIONAHA.116.021314
- Zeller CB, Appenzeller S. Cardiovascular disease in systemic lupus erythematosus: the role of traditional and lupus related risk factors. Curr Cardiol Rev 2008;4(2):116–22. https://doi.org/10.2174/157340308784245775
- Correll CU, Solmi M, Veronese N, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry 2017;16(2):163–80. https://doi.org/10.1002/wps.20420
- De Hert M, Detraux J, Vancampfort D. The intriguing relationship between coronary heart disease and mental disorders. Dialogues Clin Neurosci 2018;20(1):31–40. http://www.ncbi.nlm.nih.gov/pubmed/29946209 (last accessed 17 July 2019)
- Sacco S, Ornello R, Ripa P, et al. Migraine and risk of ischaemic heart disease: a systematic review and meta-analysis of observational studies. Eur J Neurol 2015;22(6):1001–11. https://doi.org/10.1111/ene.12701
- Adelborg K, Szépligeti SK, Holland-Bill L, et al. Migraine and risk of cardiovascular diseases: Danish population based matched cohort study. BMJ 2018;360:k96. https://doi.org/10.1136/bmj.k96
- Drager LF, McEvoy RD, Barbe F, et al. Sleep apnea and cardiovascular disease. Circulation 2017;136(19):1840–50. https://doi.org/10.1161/CIRCULATIONAHA.117.029400
- McEvoy RD, Antic NA, Heeley E, et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med 2016;375(10):919–31. https://doi.org/10.1056/NEJMoa1606599
- Cabinet Office and Department of Health and Social Care. Advancing our health: prevention in the 2020s. https://www.gov.uk/government/consultations/advancing-our-health-prevention-in-the-2020s (last accessed 28 August 2019)
- Department of Health and Social Care. Childhood obesity: a plan for action. Chapter 2. https://www.gov.uk/government/publications/childhood-obesity-a-plan-for-action-chapter-2 (last accessed 28 August 2019)
- Marteau TM, Ogilvie D, Roland M, et al. Judging nudging: can nudging improve population health? BMJ 2011;342:d228. https://doi.org/10.1136/bmj.d228
- Bramlage P, Messer C, Bitterlich N, et al. The effect of optimal medical therapy on 1-year mortality after acute myocardial infarction. Heart 2010;96(8):604–9. https://doi.org/10.1136/hrt.2009.188607
- Grace SL, Russell KL, Reid RD, et al. Effect of cardiac rehabilitation referral strategies on utilization rates. Arch Intern Med 2011;171(3):235. https://doi.org/10.1001/archinternmed.2010.501
- Powell R, McGregor G, Ennis S, et al. Is exercise-based cardiac rehabilitation effective? A systematic review and meta-analysis to re-examine the evidence. BMJ Open 2018;8(3):e019656. https://doi.org/10.1136/bmjopen-2017-019656


All rights reserved. No part of this programme may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the publishers, Medinews (Cardiology) Limited.
It shall not, by way of trade or otherwise, be lent, re-sold, hired or otherwise circulated without the publisher’s prior consent.
Medical knowledge is constantly changing. As new information becomes available, changes in treatment, procedures, equipment and the use of drugs becomes necessary. The editors/authors/contributors and the publishers have taken care to ensure that the information given in this text is accurate and up to date. Readers are strongly advised to confirm that the information, especially with regard to drug usage, complies with the latest legislation and standards of practice.
Healthcare professionals should consult up-to-date Prescribing Information and the full Summary of Product Characteristics available from the manufacturers before prescribing any product. Medinews (Cardiology) Limited cannot accept responsibility for any errors in prescribing which may occur.