Mitral regurgitation
Echocardiographic minimum dataset
The echocardiographic minimum dataset for mitral regurgitation (see figures 10–12) consist of:
- detailed description of the valve appearance and mobility (giving an assessment of aetiology and mechanism) (see table 4)
- colour mapping
- Doppler parameters (peak velocity, mean gradient)
- left atrial size
- LV geometry and function
- pulmonary artery pressure.
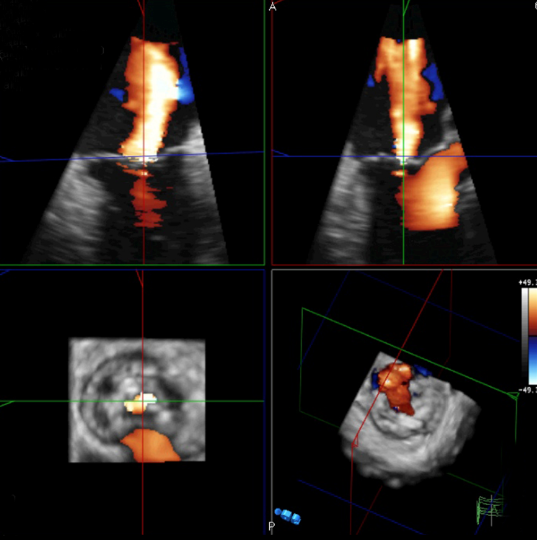
Doppler colour map
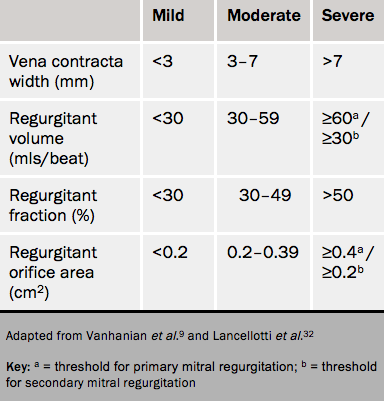
The jet consists of an intraventricular flow acceleration, a neck and the intra-atrial portion. The intra-atrial portion is easily modified by pressure and by impinging on the side of the atrium and does not give a reliable estimate of severity. However, measures related to the size of the orifice are fundamental. These are the vena contracta width and calculations using the first aliasing shell which can be used to calculate the regurgitant orifice area (ROA) and regurgitant volume (see table 5).
Spectral Doppler
Other suggestions of severe mitral regurgitation are:
- a peak transmitral velocity >1.5 m/s
- a mitral VTI: aortic VTI >1.4 (in the absence of mitral stenosis).33
Left ventricle
In severe organic regurgitation, the LV should be hyperdynamic because of volume-load. Surgery is indicated9 for:
- LVEF <60%
- LV systolic (LVS) diameter >40 mm if repairable
- LVS diameter ≥4.5 cm.
Since the LV becomes rounder in severe regurgitation, a unidimensional measure at the base of the LV may not be representative. Volumes should always be measured and the suspicion of deterioration based on linear dimensions should be corroborated by volume, Doppler tissue and sub-aortic VTI. Doppler tissue strain and strain rate imaging is expected to show early changes, but is not in clinical use.
Left atrium
This enlarges with chronic severe mitral regurgitation and is sometimes a criterion for surgery.
Grading mitral regurgitation
These quantifications are shown in table 5. Confusingly there are different cut-points for organic (primary) and functional (secondary) regurgitation. This arises because the prognostic effect of functional regurgitation is seen above ROA 20 mm2.
Advanced echocardiography
TOE is not usually needed unless there is suboptimal transthoracic imaging or unexplained discrepancies between, for example, the site of prolapse and direction of the jet.
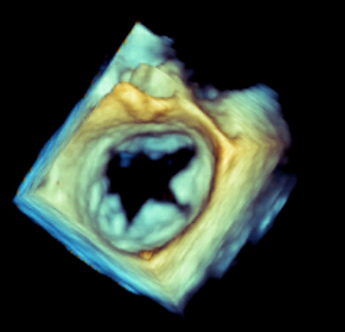
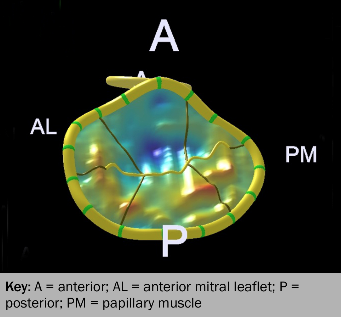
3D improves the localisation of the site of prolapse, and is particularly useful if anything more complex than prolapse of the middle scallop of the posterior leaflet is suspected.
Exercise echocardiography may be used in asymptomatic patients with severe mitral regurgitation34 or in those with discordant symptoms by providing information on:
- exercise-induced changes in mitral regurgitation35 – an exercise-induced increase in effective regurgitant orifice area (EROA) ≥13 mm2 is associated with a much worsened prognosis in those with an ischaemic aetiology of mitral regurgitation
- LV systolic function
- pulmonary artery pressure – an exercise-induced increase in pulmonary artery systolic pressure to >60 mmHg may influence the decision for mitral valve repair in selected cases (European Society of Cardiology (ESC) and American College of Cardiology (ACC)/American Heart Association (AHA) guidelines).9
Cardiac computed tomography in mitral regurgitation
In mitral regurgitation cardiac CT gives:
- the effective ROA by planimetry36 (correlates well with that measured on TEE)
- mitral annulus size
- mitral leaflets morphology and calcification
- chordal thickening
- left atrial size
- detection of pulmonary oedema.
Cardiac magnetic resonance imaging in mitral regurgitation
In mitral regurgitation CMR is not routine but can give:
- an accurate anatomical assessment of the mitral valve
- an accurate localisation of regurgitant jets37
- regurgitant volume and regurgitant fraction. Forward flow within the aorta at the level of the sinus of valsalva is measured using VENC and is subtracted from the stroke volume.