Mitral stenosis
Echocardiographic minimum dataset
The echocardiographic minimum dataset for mitral stenosis consists of:
- detailed description of the valve appearance and mobility (aetiology and mechanism)
- geometric orifice area
- mean gradient
- left atrial size
- effect on the right ventricle and pulmonary artery pressure.
Rheumatic disease causes:
- the leaflet tips to become preferentially thickened
- commissural fusion
- chordal thickening and matting.
Suitability for balloon valvotomy can be gauged by the Wilkins score38 in which a score of 1-4 is given for:
- leaflet thickening
- leaflet mobility
- leaflet calcification
- chordal involvement.
A Wilkins score >8 is unfavourable. However the commissure and chordae are the more important elements within this score and valvotomy is not usually feasible if there is one or more of the following:
- bicommissural or heavy calcification of one commissure
- heavy chordal involvement
- more than mild regurgitation
- mobile left atrial appendage thrombus.
An approximate idea of orifice area can be obtained using colour Doppler. However, planimetry should be attempted using the parasternal short axis on a mid-diastolic frame and a zoomed in view.2 This is facilitated by 3D.39
Grading mitral stenosis (see table 6)
When grading mitral stenosis, the geometric orifice area is the predominant measure. An indirect measure of area is obtained using the pressure T1/2:40
MVA = 220/ T1/2
(where MVA = mitral valve area)
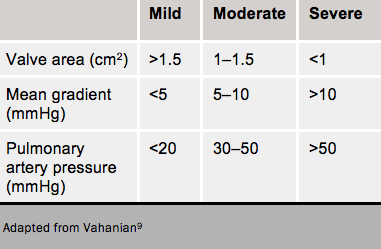
This gives only an approximate relationship with area and is particularly inaccurate in mild stenosis or after balloon valvotomy. Mean gradient is dependent on flow (see table 6).
Where there are discrepancies between the planimetered and CW Doppler measurements of stenosis severity, other measurements using the continuity equation and proximal isovelocity surface area methods are recommended, although not generally necessary or widely used.
Advanced echocardiography
3D is increasingly useful to guide planimetry of the orifice which may often be out of the plane of a conventional 2D section.39
TOE is essential before balloon valvotomy to exclude mobile left atrial appendage thrombus, and confirm the other TTE findings.
Stress echocardiography is useful in patients with uncertain symptoms34 looking for:
- An increase in mean gradient to >15 mmHg
- A rise in pulmonary arterial systolic pressure to >60 mmHg
- LV decompensation as a result of coexistent coronary disease.
Cardiac computed tomography in mitral stenosis
For an evaluation of the valve components, a reconstruction at 65% of the R-R interval for the open mitral valve, and a reconstruction at 5% of the R-R interval is recommended for the closed mitral valve.
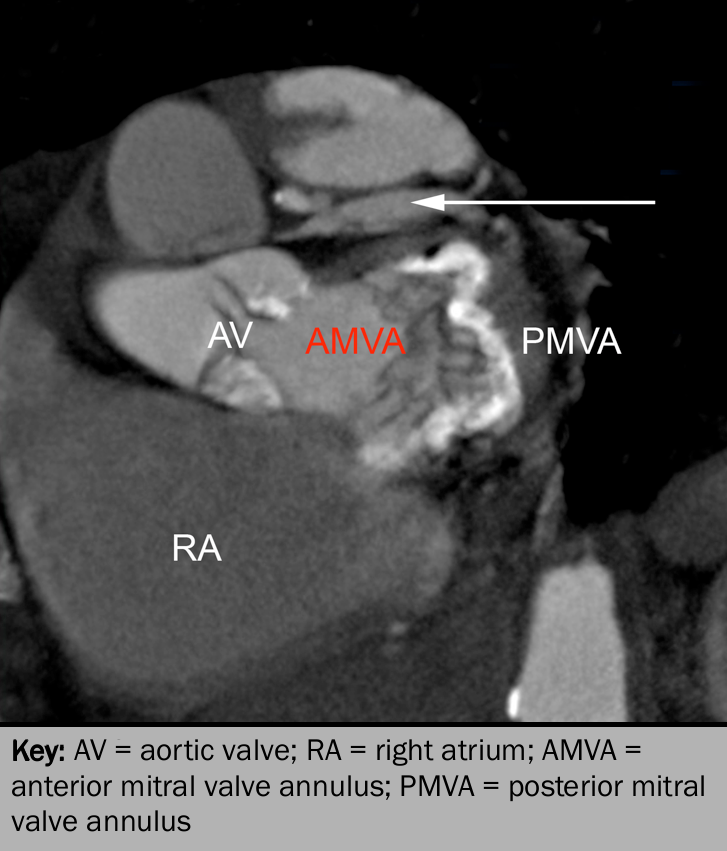
In mitral stenosis, CT may be useful for:
- excellent anatomical and morphological detail of the mitral valve apparatus
- detection of calcium in leaflet, commissure and annulus (see figure 13)
- geometric orifice by direct planimetry (correlates well with TEE findings (R=0.88, p<0.001))41
- accurate left atrial size
- detection of left atrial thrombus
- right ventricular hypertrophy
- radiographic evidence of pulmonary oedema and pulmonary hypertension.
Cardiac magnetic resonance imaging in mitral stenosis
CMR imaging may be used for the assessment of mitral stenosis but is considered to be a second-line technique for this purpose. Much as with the aortic valve, mitral inflow turbulence may be seen on SSFP in-plane imaging and the mitral valve area may be measured using carefully placed through plane SSFP imaging. Although this technique has been shown to correlate well with echo derived areas,42–3 it is often limited by the presence of atrial fibrillation and problems with electrocardiogram (ECG)-gating.
