The ESC guidelines recommend prophylaxis for high risk patients undergoing the highest risk procedures.42 The patients at highest risk are those who have previously had endocarditis, those with a prosthetic valve, uncorrected or only partially corrected cyanotic congenital heart disease, corrected congenital heart disease in the first six months after surgery, and those with a residual defect at the site of prosthetic material. The highest risk procedures are “dental procedures requiring manipulation of the gingival or periapical region of the teeth or perforation of the oral mucosa” (which includes dental scaling). Amoxicillin or ampicillin are the recommended prophylactic antibiotics – clindamycin may be used in those with penicillin allergy.
Patients at high risk undergoing non-high risk procedures (such as bronchoscopy or colonoscopy) do not require antibiotic prophylaxis. Similarly, patients with non-high risk heart disease (such as mitral valve prolapse) undergoing high risk procedures should not receive antibiotic prophylaxis.
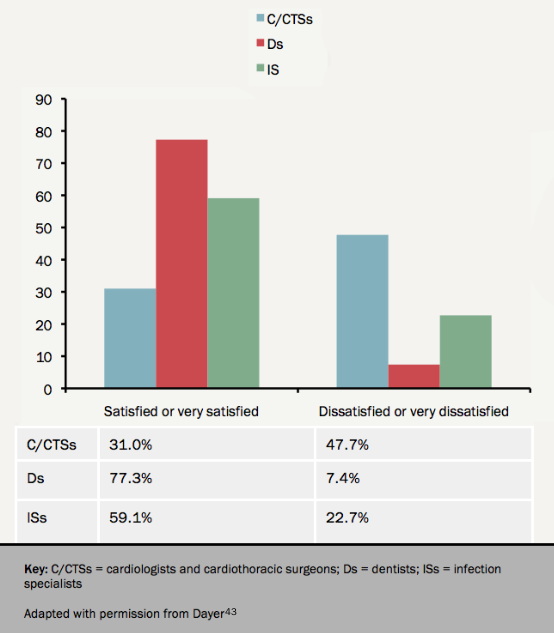
In contrast, the UK National Institute for Health and Clinical Excellence (NICE) recommends that antibiotic prophylaxis is not indicated for any patient in any situation. This controversial recommendation has the advantage of removing the uncertainty and variability between clinical practitioners in interpretation of the international guidelines (see figure 943). Nevertheless, the views of NICE are not supported by a significant number of cardiologists and cardiac surgeons.44 The sharp reduction in prophylactic antibiotic prescribing following the introduction of the NICE guidelines was accompanied by an increase in trend of incidence of endocarditis in the UK.45 In the absence of randomised trial evidence, this cotroversy is unlikely to be further clarified in the near future.
Conclusions
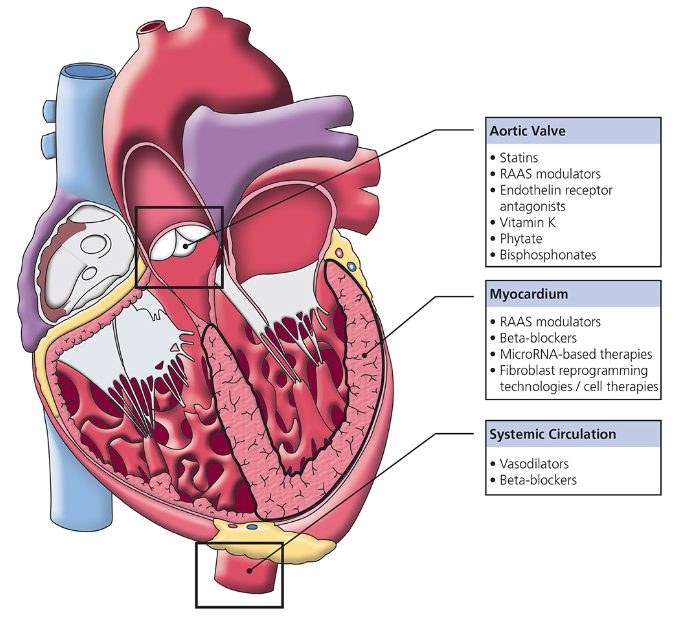
In this module we have discussed disease-modifying and supportive medical therapy for patients with VHD (see figure 10), indications for anticoagulation in patients with native VHD, and antibiotic prophylaxis of endocarditis. Disease-modifying treatments have not provided the anticipated clinical outcomes, while previous dogma around supportive therapy (such as the avoidance of vasodilators in patients with AS) has been recently challenged. Over the next decade, we hope that new evidence will enlighten our decision making in the pharmacological treatment of VHD.
close window and return to take test
References
1 Cowell SJ, Newby DE, Prescott RJ, et al. A randomized trial of intensive lipid-lowering therapy in calcific aortic stenosis. N Engl J Med 2005;352:2389–97. http://dx.doi.org/10.1056/NEJMoa043876
2 Rossebø AB, Pedersen TR, Boman K, et al. Intensive lipid lowering with simvastatin and ezetimibe in aortic stenosis. N Engl J Med 2008;359:1343–56. http://dx.doi.org/10.1056/NEJMoa0804602
3 Chan KL, Teo K, Dumesnil JG, et al. Effect of Lipid lowering with rosuvastatin on progression of aortic stenosis: results of the aortic stenosis progression observation: measuring effects of rosuvastatin (ASTRONOMER) trial. Circulation 2010;121:306–14. http://dx.doi.org/10.1161/CIRCULATIONAHA.109.900027
4 Helske S, Lindstedt K a, Laine M, et al. Induction of local angiotensin II-producing systems in stenotic aortic valves. J Am Coll Cardiol 2004;44:1859–66. http://dx.doi.org/10.1016/j.jacc.2004.07.054
5 Arishiro K, Hoshiga M, Negoro N, et al. Angiotensin receptor-1 blocker inhibits atherosclerotic changes and endothelial disruption of the aortic valve in hypercholesterolemic rabbits. J Am Coll Cardiol 2007;49:1482–9. http://dx.doi.org/10.1016/j.jacc.2006.11.043
6 Ngo DT, Stafford I, Sverdlov AL, et al. Ramipril retards development of aortic valve stenosis in a rabbit model: mechanistic considerations. Br J Pharmacol 2011;162:722–32. http://dx.doi.org/10.1111/j.1476-5381.2010.01084.x
7 Pope M, McIntyre H. News from the 7th annual scientific meeting of the Cardiorenal Forum. Br J Cardiol 2013;20:20–1.
8 Nadir MA, Wei L, Elder DHJ, et al. Impact of renin-angiotensin system blockade therapy on outcome in aortic stenosis. J Am Coll Cardiol 2011;58:570–6. http://dx.doi.org/10.1016/j.jacc.2011.01.063
9 Olsen MH, Wachtell K, Bella JN, et al. Effect of losartan versus atenolol on aortic valve sclerosis (a LIFE substudy). Am J Cardiol 2004;94:1076–80. http://dx.doi.org/10.1016/j.amjcard.2004.06.074
10 Azevedo CF, Nigri M, Higuchi ML, et al. Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. J Am Coll Cardiol 2010;56:278–87. http://dx.doi.org/10.1016/j.jacc.2009.12.074
11 Stewart RAH, Kerr AJ, Cowan BR, et al. A randomized trial of the aldosterone-receptor antagonist eplerenone in asymptomatic moderate-severe aortic stenosis. Am Heart J 2008;156:348–55. http://dx.doi.org/10.1016/j.ahj.2008.03.012
12 Bull S, Loudon M, Francis JM, et al. A prospective, double-blind, randomized controlled trial of the angiotensin-converting enzyme inhibitor Ramipril In Aortic Stenosis (RIAS trial). Eur Heart J Cardiovasc Imaging 2015;16:834–41. http://dx.doi.org/10.1093/ehjci/jev043
13 Varadarajan P, Kapoor N, Bansal RC, et al. Clinical profile and natural history of 453 nonsurgically managed patients with severe aortic stenosis. Ann Thorac Surg 2006;82:2111–5. http://dx.doi.org/10.1016/j.athoracsur.2006.07.048
14 Desai PA, Tafreshi J, Pai RG. Beta-blocker therapy for valvular disorders. J Heart Valve Dis 2011;20:241–53.
15 Chockalingam A, Venkatesan S, Subramaniam T, et al. Safety and efficacy of angiotensin-converting enzyme inhibitors in symptomatic severe aortic stenosis: Symptomatic Cardiac Obstruction-Pilot Study of Enalapril in Aortic Stenosis (SCOPE-AS). Am Heart J 2004;147:E19. http://dx.doi.org/10.1016/j.ahj.2003.10.017
16 Dalsgaard M, Iversen K, Kjaergaard J, et al. Short-term hemodynamic effect of angiotensin-converting enzyme inhibition in patients with severe aortic stenosis: a placebo-controlled, randomized study. Am Heart J 2014;167:226–34. http://dx.doi.org/10.1016/j.ahj.2013.11.002
17 Lindman BR, Zajarias A, Madrazo J a, et al. Effects of phosphodiesterase type 5 inhibition on systemic and pulmonary hemodynamics and ventricular function in patients with severe symptomatic aortic stenosis. Circulation 2012;125:2353–62. http://dx.doi.org/10.1161/CIRCULATIONAHA.111.081125
18 Khot UN, Novaro GM, Popović ZB, et al. Nitroprusside in critically ill patients with left ventricular dysfunction and aortic stenosis. N Engl J Med 2003;348:1756–63. http://dx.doi.org/10.1056/NEJMoa022021
19 Scognamiglio R, Rahimtoola SH, Fasoli G, et al. Nifedipine in asymptomatic patients with severe aortic regurgitation and normal left ventricular function. N Engl J Med 1994;331:689–94. http://dx.doi.org/10.1056/NEJM199409153311101
20 Evangelista A, Tornos P, Sambola A, et al. Long-term vasodilator therapy in patients with severe aortic regurgitation. N Engl J Med 2005;353:1342–9. http://dx.doi.org/10.1056/NEJMoa050666
21 Shah RM, Singh M, Bhuriya R, et al. Favorable effects of vasodilators on left ventricular remodeling in asymptomatic patients with chronic moderate-severe aortic regurgitation and normal ejection fraction: a meta-analysis of clinical trials. Clin Cardiol 2012;35:619–25. http://dx.doi.org/10.1002/clc.22019
22 Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012): The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2012;33:2541–96. http://dx.doi.org/10.1093/eurheartj/ehs109
23 Sampat U, Varadarajan P, Turk R, et al. Effect of beta-blocker therapy on survival in patients with severe aortic regurgitation results from a cohort of 756 patients. J Am Coll Cardiol 2009;54:452–7. http://dx.doi.org/10.1016/j.jacc.2009.02.077
24 Stewart RAH, Raffel OC, Kerr AJ, et al. Pilot study to assess the influence of beta-blockade on mitral regurgitant volume and left ventricular work in degenerative mitral valve disease. Circulation 2008;118:1041–6. http://dx.doi.org/10.1161/CIRCULATIONAHA.108.770438
25 Ahmed MI, Aban I, Lloyd SG, et al. A randomized controlled phase IIb trial of beta(1)-receptor blockade for chronic degenerative mitral regurgitation. J Am Coll Cardiol 2012;60:833–8. http://dx.doi.org/10.1016/j.jacc.2012.04.029
26 Strauss CE, Duval S, Pastorius D, et al. Pharmacotherapy in the treatment of mitral regurgitation: a systematic review. J Heart Valve Dis 2012;21:275–85.
27 Marijon E, Mirabel M, Celermajer DS, et al. Rheumatic heart disease. Lancet 2012;379:953–64. http://dx.doi.org/10.1016/S0140-6736(11)61171-9
28 Meister SG, Engel TR, Feitosa GS, et al. Propranolol in mitral stenosis during sinus rhythm. Am Heart J 1977;94:685–8. http://dx.doi.org/10.1016/S0002-8703(77)80207-X
29 Klein HO, Sareli P, Schamroth CL, et al. Effects of atenolol on exercise capacity in patients with mitral stenosis with sinus rhythm. Am J Cardiol 1985;56:598–601. http://dx.doi.org/10.1016/0002-9149(85)91018-5
30 Stoll BC, Ashcom TL, Johns JP, et al. Effects of atenolol on rest and exercise hemodynamics in patients with mitral stenosis. Am J Cardiol 1995;75:482–4. http://dx.doi.org/10.1016/S0002-9149(99)80585-2
31 Bassan MM, Michaeli J, Shalev O. Failure of propranolol to improve exercise tolerance in patients with mitral stenosis in sinus rhythm. Br Heart J 1987;58:254–8. http://dx.doi.org/10.1136/hrt.58.3.254
32 Patel JJ, Dyer RB, Mitha AS. Beta adrenergic blockade does not improve effort tolerance in patients with mitral stenosis in sinus rhythm. Eur Heart J 1995;16:1264–8.
33 Misra M, Bhandari K, Thakur R, et al. Failure of oral atenolol and verapamil to increase the capacity and duration of exercise in patients in sinus rhythm with mitral stenosis. Int J Cardiol 1989;23:37–41. http://dx.doi.org/10.1016/0167-5273(89)90327-6
34 Alan S, Ulgen MS, Ozdemir K, et al. Reliability and efficacy of metoprolol and diltiazem in patients having mild to moderate mitral stenosis with sinus rhythm. Angiology 2002;53:575–81. http://dx.doi.org/10.1177/000331970205300512
35 Parakh N, Chaturvedi V, Kurian S, et al. Effect of ivabradine vs atenolol on heart rate and effort tolerance in patients with mild to moderate mitral stenosis and normal sinus rhythm. J Card Fail 2012;18:282–8. http://dx.doi.org/10.1016/j.cardfail.2012.01.001
36 Otto CM, Lind BK, Kitzman DW, et al. Association of aortic-valve sclerosis with cardiovascular mortality and morbidity in the elderly. N Engl J Med 1999;341:142–7. http://dx.doi.org/10.1056/NEJM199907153410302
37 De Caterina R, Camm AJ. What is ‘valvular’ atrial fibrillation? A reappraisal. Eur Heart J 2014;35:3328-35. http://dx.doi.org/10.1093/eurheartj/ehu352
38 Avezum A, Lopes RD, Schulte PJ, et al. Apixaban in Comparison With Warfarin in Patients With Atrial Fibrillation and Valvular Heart Disease: Findings From the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) Trial. Circulation 2015;132:624-32. http://dx.doi.org/10.1161/CIRCULATIONAHA.114.014807
39 Heidbuchel H, Verhamme P, Alings M, et al. Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace 2015 Aug 31. [Epub ahead of print] http://dx.doi.org/10.1093/europace/euv309
40 Breithardt G, Baumgartner H, Berkowitz SD, et al. Clinical characteristics and outcomes with rivaroxaban vs. warfarin in patients with non-valvular atrial fibrillation but underlying native mitral and aortic valve disease participating in the ROCKET AF trial. Eur Heart J 2014;35:3377-85. http://dx.doi.org/10.1093/eurheartj/ehu305
41 Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med 2009;169:463–73. http://dx.doi.org/10.1001/archinternmed.2008.603
42 Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC)Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015 Aug 29. [Epub ahead of print] http://dx.doi.org/10.1093/eurheartj/ehv319
43 Dayer MJ, Chambers JB, Prendergast B, Sandoe JAT, Thornhill MH. NICE guidance on antibiotic prophylaxis to prevent infective endocarditis: a survey of clinicians’ attitudes. QJM 2013; http://dx.doi.org/10.1093/qjmed/hcs235
44 Chambers JB, Shanson D, Hall R, et al. Antibiotic prophylaxis of endocarditis: the rest of the world and NICE. J R Soc Med 2011;104:138–40. http://dx.doi.org/10.1258/jrsm.2011.100356
45 Dayer MJ, Jones S, Prendergast B, et al. Incidence of infective endocarditis in England, 2000-13: a secular trend, interrupted time-series analysis. Lancet 2015;385:1219-28. http://dx.doi.org/10.1016/S0140-6736(14)62007-9
close window and return to take test
All rights reserved. No part of this programme may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the publishers, Medinews (Cardiology) Limited.
It shall not, by way of trade or otherwise, be lent, re-sold, hired or otherwise circulated without the publisher’s prior consent.
Medical knowledge is constantly changing. As new information becomes available, changes in treatment, procedures, equipment and the use of drugs becomes necessary. The editors/authors/contributors and the publishers have taken care to ensure that the information given in this text is accurate and up to date. Readers are strongly advised to confirm that the information, especially with regard to drug usage, complies with the latest legislation and standards of practice.
Healthcare professionals should consult up-to-date Prescribing Information and the full Summary of Product Characteristics available from the manufacturers before prescribing any product. Medinews (Cardiology) Limited cannot accept responsibility for any errors in prescribing which may occur.
