Despite documented evidence of benefits of lifestyle cardioprotective interventions in reducing recurrent coronary heart disease (CHD) events, many patients still fail to adhere to proposed lifestyle interventions. To determine the percentage adherence rate and to identify the perceived barriers influencing adherence rate to cardioprotective lifestyle interventions among patients treated with primary percutaneous coronary intervention (PPCI) a cross-sectional survey was designed.
A total of 193 consecutive patients, with a clinical diagnosis of CHD who had a PPCI, were identified retrospectively between 2008 and 2013, and were subsequently telephone surveyed. Data were analysed using chi-square tests and Fisher’s exact tests. At survey, 21.8% of patients smoked cigarettes, 30.6% were adhering to physical activities as per guidelines, 36.3% were consuming five portions of fruits and vegetables per day, and 9.8% were consuming three portions of oily fish per week. Negative stress, low mood, advanced age, poor health, lack of enjoyment from physical activities, low expectations from physical activity benefits, obesity and diabetes, were associated with non-adherence to physical activities as per guidelines.
In conclusion, risk factor targets for secondary prevention were not reached by a large proportion of patients. Several barriers exist among these individuals. Thus, there is still considerable potential for cardiac rehabilitation clinicians to improve standards of preventive cardiology by clearly identifying barriers and ways to overcome them.

Introduction
Cardiovascular disease (CVD) remains a major cause of mortality worldwide, with 3.9 million deaths per year in Europe attributed to this disease.1 Optimal behavioural modifications of lifestyle risk factors in patients with established coronary heart disease (CHD) have been significantly associated with prevention of recurrent coronary atherosclerotic events.2 For this reason the joint task force of the European Society of Cardiology and other societies (JES5)3 have put emphasis on preventive cardiology lifestyle interventions, which are smoking cessation, making healthy food choices and contribution to moderate intensity aerobic exercises of ≥3 times a week, of 30 minutes per session. However, the extent to which preventive cardiology lifestyle interventions are effective, are dependent on patient’s adherence to these interventions.2,4-6
The JES53 have described assessment, targets and management strategies of modifiable cardiovascular (CV) risk factors, putting emphasis on exercise, diet, and smoking. Thus, the aim of this cross-sectional study was to estimate the percentage adherence and the association of patient-reported perceived barriers to lifestyle interventions, one to six years after being treated with primary percutaneous coronary intervention (PPCI).
Method
Design and setting
This was a cross-sectional survey study of a population consisting of patients who had a PPCI. The study was conducted in a small developed country with an adult population of 310,819.7 This country has only one acute general state hospital. Casualties presenting with ST-segment elevation myocardial infarction (STEMI) are treated with a PPCI at the catheterisation-lab and transferred to the cardiac critical care unit (CCCU). Consecutive patients admitted from March 2008 to March 2013 were retrospectively selected from CCCU electronic data (cardiovascular information system). This electronic system was introduced to our hospital in 2008, therefore, patients from previous years were not included.
Sample
Eligible research subjects, were patients diagnosed with STEMI. This was confirmed via biochemistry reports (positive significant troponin I, cut-off point 0.04 ng/ml) and catheterisation laboratory reports. Only patients who had evidence of a culprit lesion that needed a primary stent deployment were enrolled. Exclusion criteria included patients with non-ST-segment elevation acute coronary syndrome and patients who had a positive troponin I, but no evidence of a coronary culprit lesion, therefore, not needing a stent. In total, 338 selected patients were found to be eligible for the survey questionnaire. A sample of 193 patients were successfully recruited to take part in this study. Using a sample calculator based on a population of 112,000 individuals with established CHD, guaranteed a maximum margin of error of 7.05%, assuming a 95% confidence level (CI). In other words, the sample size calculation proved that data from 193 individuals are sufficient to estimate adherence with a precision of at least 5.0% and a 95% CI. The study was approved by the data protection unit of the hospital and was carried out in accordance with the requirements of the Data Protection Act (Chap. 440). A third person contacted the eligible patients (n=338), and obtained verbal consent after giving a brief description of the study. Those who gave permission were contacted by the researcher and provided their information through a telephone-based questionnaire.
Data collection
Adherence and barrier score assessment
Data collection was carried out from April 2013 to August 2013. Data from participant’s questionnaires, including demographic details, family history of CVD, access to cardioprotective counselling, and adherence to lifestyle interventions about smoking, diet and physical exercise, were assessed. To determine participants’ percentage adherence, concise questions based on JES5 lifestyle targets were used.3 Patients were defined as being adherent, if they were found to be corresponding with lifestyle targets as defined by JES5 guidelines.3 All patients who were not corresponding with the lifestyle targets, were considered as being non-adherent to guidelines. A list of possible barriers was included in the survey questionnaire where patients had to report whether these factors were personally impeding adherence to smoking cessation (for continued smokers), physical activity target and maintaining healthy food choices.
Data analysis
All statistical analyses were undertaken using SPSS 19.0 (SPSS Inc., Chicago, Illinois, USA). As this was a descriptive survey, with emphasis on estimation of adherence and associated perceived barriers, no formal hypothesis testing was done. In the case for categorical variables, the Pearson chi-square test and the Fisher’s exact test were computed to determine whether an association was present between adherence to guidelines and existing barriers. A p value <0.05 indicated that the association was statistically significant. For continuous variables the means and standard deviation (SD) are displayed to measure central tendency and dispersion. The mean overall (percentage) adherence to at least one guideline was calculated by averaging the percentage adherence of all seven guideline targets.
Rigour
The tool was originally developed for the purpose of this study. The tool was piloted on a sample of 25 PPCI patients that were randomly selected from the 2006 CCCU archive. This ascertained that the questionnaire is satisfactory with length, flow and clarity. The tool showed good reliability with the intraclass method, with a 0.976 correlation coefficient (95% CI, range 0.961–0.982).
Results
Response: characteristics of the study participants
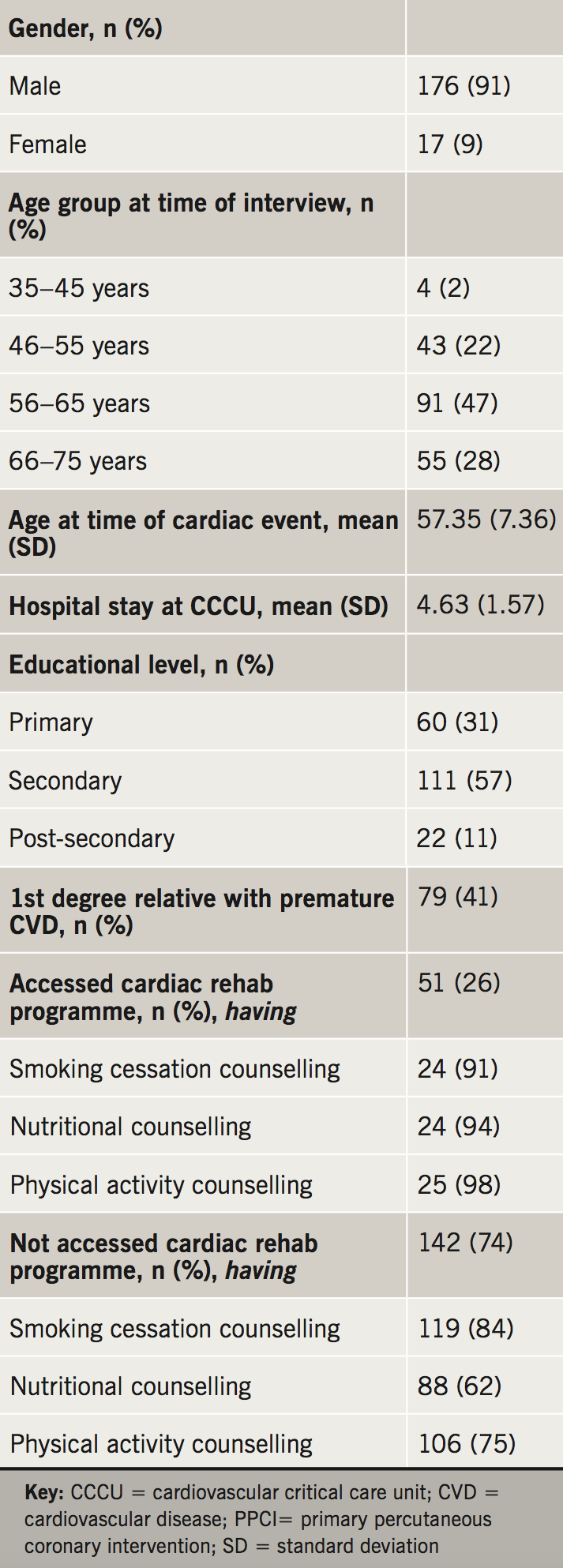
Characteristics of this study population and access to cardioprotective counselling are shown in table 1. From 338 selected participants, 64 refused to participate (18.9%) and 81 were unreachable despite numerous attempts at contacting them (23.9%). This provides a response rate of 57.2% (n=193). The mean age at time of cardiac event among participants in this study was 57.35 years (range 35 to 71 years), and the majority were male (91.2%, n=176). The majority completed primary and secondary education (88.6%), while only 11.4% had post-secondary education. First-degree relatives with premature CVD (male <55, female <65 years) was reported in 40.9% of cases. Additionally, a minimal number of participants attended the full one-year follow-up cardiac rehabilitation program (CRP) (26.4%).
Percentage adherence to cardioprotective lifestyle
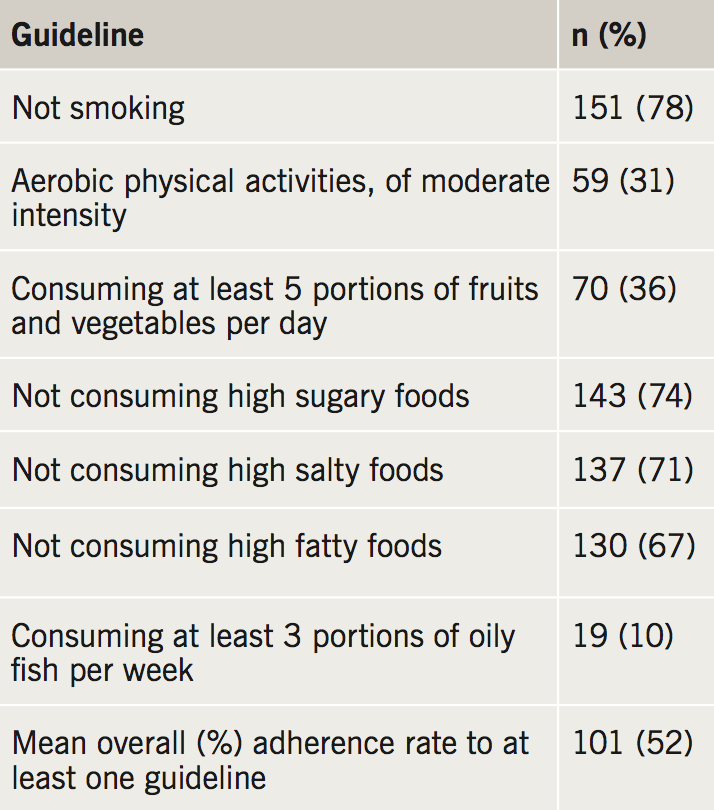
Table 2 represents the proportion of adherence to cardioprotective targets among all participants. A large proportion of participants (n=133) reported that they were smokers prior to their cardiac event, with a mean of 37.5 smoking years (SD ±10.113). Smoking following PPCI was reported among 31.6% (n=42), with an average of 13 cigarettes per day. Of those still smoking during the time of survey, 90.5% reported that they ‘really tried quitting’. Despite this, smoking cessation aids were barely used among smokers (13.5%). Regarding physical activities, the majority of participants (69.4%) considered themselves to be physically active. However, only 30.6% were adherent to physical activity as recommended by the JES5. When asked about healthy food choices, in all, 29%, 32.6% and 25.9% were consuming foods that are high in salt content, saturated/trans fats, and sugar content, respectively. Moreover, 36.3% stated that they were getting the daily recommended intake of fruit and vegetables and 9.8% the recommended weekly intake of oily fish. The impact of time on percentage adherence post-PPCI to not smoking and physical activity, as per JES5 guidelines, was determined between the five subgroups (1–2 years, 2–3 years, 3–4 years, 4–5 years, 5–6 years post-PPCI). However, the trend of time post-PPCI between subgroups was not significant (p=0.095, p=0.397).
Barriers influencing adherence to guidelines
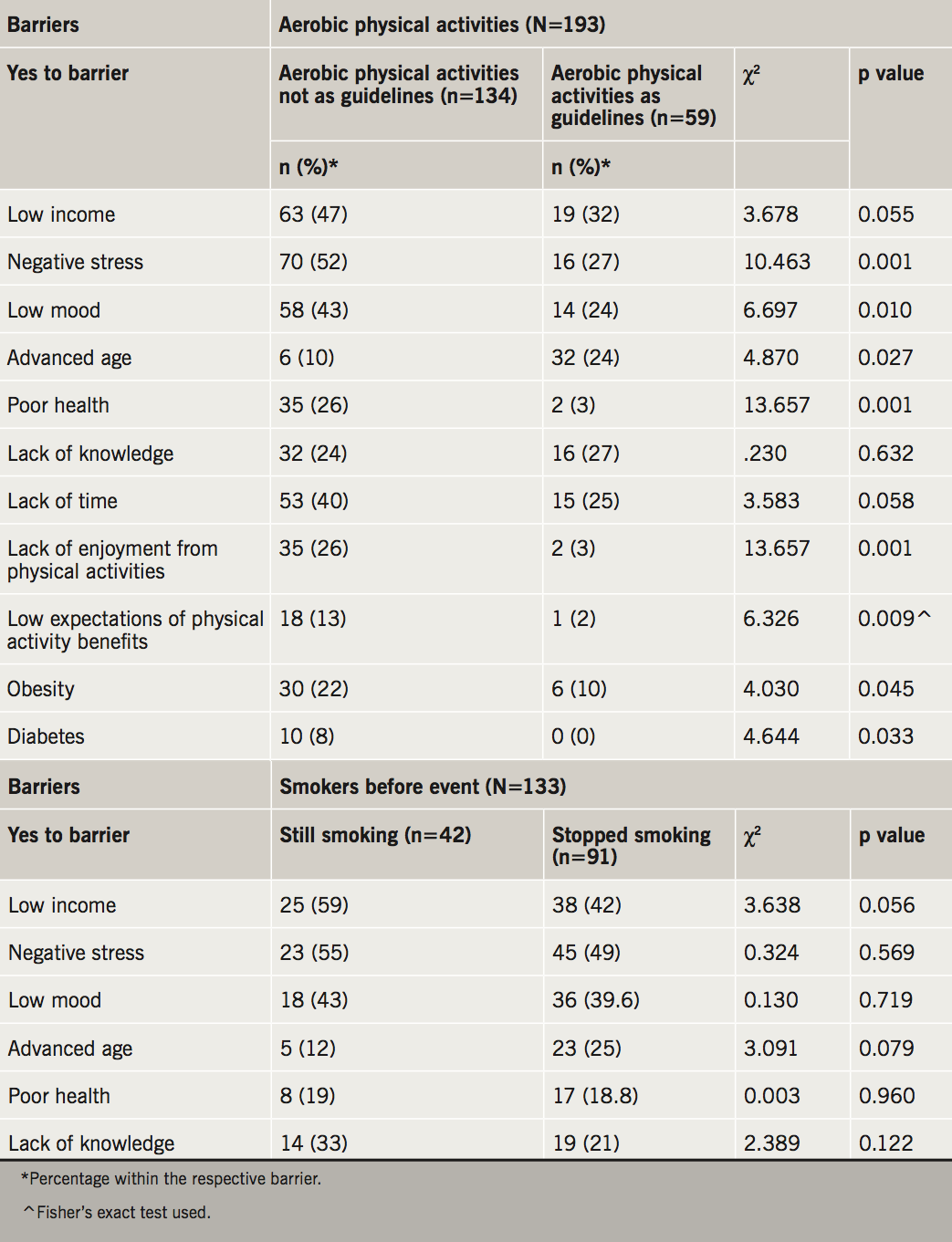
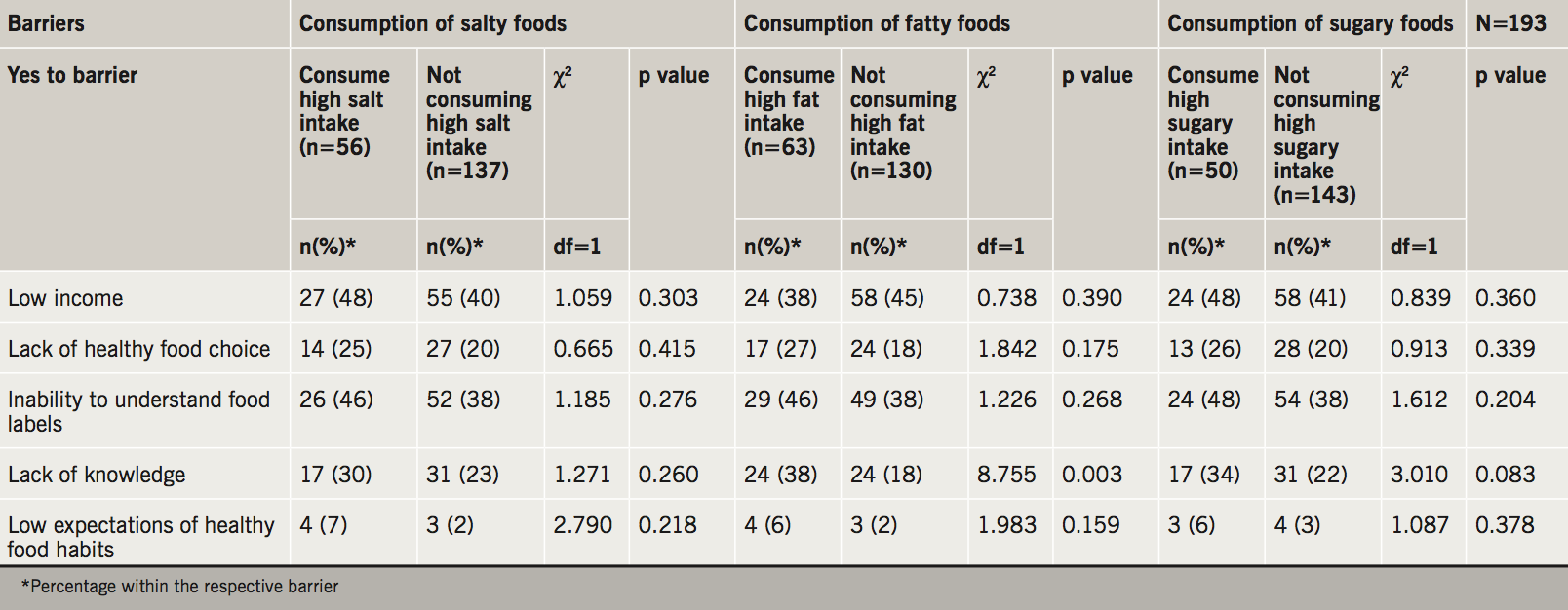
In the second step, the study investigated the perceived barriers and their association to cardioprotective lifestyle interventions. There was no statistically significant association between perceived barriers to smoking and failure to quit smoking (table 3). As seen in table 3, of all variables included, negative stress (p=0.001), low mood (p=0.010), advanced age (p=0.027), poor health (p=0.001), lack of enjoyment from physical activities (p=0.001), as well as low expectations of physical activity benefits (p=0.012), obesity (p=0.045) and diabetes (p=0.031) were significantly associated with low percentage adherence to aerobic physical activities as per JES5 guidelines. Lack of knowledge was the only barrier that showed a statistically significant association with consumption of high saturated/trans fatty foods (table 4). No barrier association was noted to food consumption as per guidelines.
Discussion
Percentage adherence to cardioprotective lifestyle
The present study was designed to estimate percentage adherence to cardioprotective lifestyle interventions among PPCI patients, and also to investigate which factors could influence percentage adherence. The main findings of this study revealed that many patients fail to adhere to cardioprotective lifestyle measures. In fact, the average of total percentage adherence to at least one of the seven goals assessed (table 2) among study participants amounted to only 52.5%. Similarly, the EuroAspire surveys (2009) have demonstrated that a large gap exists between reality and the ideal adherence to the three basic lifestyle behaviours, namely the uptake of regular physical activity, smoking avoidance, and eating a healthy diet.8
The findings of this study show that from a total of 133 smokers (before PPCI), 31.6% were still smoking at the time of survey. This compares well to other studies; Teo et al. (2013) reported a percentage of 18.5% of continued smokers,9 and other studies have reported a percentage of 40–60% of continued smokers after six months. Nonetheless, up to 70% of patients are at risk of relapse in the following year. Furthermore, reports have shown that even years after smoking abstinence, there is still a 10% risk of a future relapse. Researchers argue that relapses could be linked to the various demographic origins, apart from being influenced by the level of nicotine dependence and psychosocial factors, namely depression. In the present study, low mood was perceived as a personal barrier in 40.6% (n=54) of those who smoked before the event (n=133), of whom 43% (n=23) were unsuccessful quitters. The majority of unsuccessful quitters admitted that they tried their utmost to quit (90.5%), however, no recognised barriers were found to be associated with continued smoking. The obtained results indicate that understanding the perceived barriers associated with unsuccessful quitting is complex, but one cannot exclude the possibility of high nicotine dependence among participants. Yet, smoking cessation aids, such as nicotine replacement therapy or varenicline, were barely used (n=18, 13.5%). This might have further improved smoking cessation results, as reported in other studies.10-13
This study has also shown that a large proportion (69.4%) of patients considered themselves as being physically active. However, only a small percentage of participants (30.6%) adhered to the recommended physical activity guidelines proposed by JES5.3 This discrepancy could be due to their involvement in mild-intensity physical activities (such as easy walking and slow dancing; 28.5%), or moderate (e.g. fast walking and easy swimming; 51.8%) physical activity, which do not comply with the JES5 physical activity target. In addition, several barriers were noticed among the study participants (table 3). We believe that these have induced a negative impact on adherence to physical activities as per guidelines.3
Regarding diet, results showed only 36.3% were consuming an average of five servings of fruit and vegetables per day. In all, 29%, 32%, and 25.9% of participants reported consuming high salt content foods, high saturated/trans fatty content foods and high sugar content foods, respectively. Similarly, DeBoer et al. (2003) observed that only 16% of adults consumed the recommended daily intake of five servings of fruits and vegetables a day.14 Furthermore, the estimated proportion of the recommended intake of fish among study participants was also low (9.8%). This could be due to globalisation of food systems, which took place over the years due to ‘McDonaldisation’, thus conditioning the population to abandon the traditional healthy Mediterranean diet.
Barriers influencing adherence to cardioprotective lifestyle targets
As shown in table 3 and table 4, results indicate that a wide array of recognised barrier variables were associated with non-adherence to physical activities as per JES5 guidelines,3 but not with smoking cessation and diet. Lack of knowledge was the only barrier that was significantly associated with consumption of high trans/saturated food-content (p<0.003) as similarly shown in the EPIC (European Prospective Investigation into Cancer and Nutrition) study.15 Other studies have also shown that socioeconomic factors, such as low income, may hinder individuals from adhering to lifestyle interventions.15,16 Low income was the second most frequently reported barrier among participants. Nonetheless, no statistically significant association was observed between low income and adherence to any of the studied targets.
Several perceived barriers were associated with poor adherence to physical activity (table 3), including negative stress (52%, n=70), and low mood (43%, n=58), advanced age (10.2%, n=6) and poor health (26%, n=35) were barriers that impeded participants from adhering to JES5 physical activity targets. This is in line with other studies reporting an age-related decline in physical activity among older individuals,17 and a positive correlation between severity of illness and physical activity.18 Lack of enjoyment from physical activity was also linked to poor physical activity adherence (26%, n=35) which is in line with other studies.19 Low expectations of physical activity benefits was also associated with poor adherence (13%, n=18). Furthermore, a lack of understanding of the benefits associated with physical activity was also reported to lead to low adherence, particularly in individuals of a low socioeconomic status.20
Although anthropometric measurements were not recorded in this study, 18.7% of PPCI patients reported obesity as a personal barrier to physical activity. Participation in aerobic physical activities was significantly poorer in obese and overweight individuals as opposed to research subjects who did not perceive their weight as a barrier. Research has shown that psychological and physiological problems are more common among obese individuals, leading to further strain on adherence.21
Poor control of diabetes may interfere with patients’ functioning and quality of life.22 In the present study, participants who reported diabetes as a personal recognised barrier (4.7%, n=10), did not adhere to physical activities as per guidelines (p<0.031), possibly due to multiple co-existing chronic diseases.23 Such diseases may adversely increase levels of psychological and physiological strain on the individual leading to an overall poorer adherence to physical activity.22
Limitations of the study
Some study limitations need to be considered. First the study results are only applicable in individuals who had a PPCI. Also results are not generalisable to other contexts due to differences in cultures, although results conform to similar studies conducted in other developed countries. Since data collected were based on self-reported measures, there is a possibility of social desirability bias, therefore, underestimating unhealthy behaviours. As results were obtained via a cross-sectional research design, causal relationships could not be inferred. However, such a design was adequate for obtaining very useful data, giving a better reflection of the real lifestyle situation among PPCI patients. Indeed, if the sample size was larger, this would have reduced the margin of error, however, due to time constraints and difficulties accessing/contacting patients the target sample was not reached. An important strength of this survey is that it shows that lifestyle modification is complex to reach and maintain. Further research on a larger scale is needed to understand this still remaining phenomenon.
Conclusion
The focus of this article was to determine the percentage adherence rate among PPCI patients to cardioprotective lifestyle targets based on the JES5 guidelines. Cardioprotective lifestyle targets for secondary prevention were not adequately met by a large proportion of patients. Overall, this survey showed that several barriers, namely; negative stress, low mood, advanced age, poor health, lack of enjoyment from physical activities, low expectations from physical activity benefits, obesity and diabetes, may impede adherence to the proposed JES5 lifestyle targets. Thus, there is still considerable potential for cardiac rehabilitation clinicians to improve standards of preventive cardiology by clearly identifying barriers and ways how to support patients to overcome them.
Relevance to clinical practice
Cardiac rehabilitation clinicians should put emphasis on patient barrier risk assessment, devise tailor-made interventions and follow-up individually. Moreover, the cardiac rehabilitation programme content should give importance to patients’ perception of the associated risks,24 be informative, including practical training and self-activities on all lifestyle factors25 to enhance self-care optimisation. These aforementioned points may help in developing better preventive strategies. This may help to improve adherence to the JES5 targets more effectively, exerting beneficial effects to reduce future atherosclerotic events.
Key messages
- There is a need to put early emphasis on patients’ barrier risk assessment to clearly identify barriers in a timely manner, devise tailor-made interventions and follow-up individually
- Cardiac rehabilitation clinicians may improve the standards of preventive cardiology by developing ways to promote healthy lifestyle interventions and make the cardiac rehabilitation programme more accessible
- Understanding behaviour to lifestyle modification is complex and further research on a larger scale is needed to understand this still remaining phenomenon
Acknowledgements
The author would like to particularly thank Dr Liberato Camilleri for help related to statistical analysis of the data; Dr Catriona Jennings, Dr Melissa Formosa and Dr Mark Sammut for their technical and writing assistance for publication.
Conflict of interest
None declared.
References
1. Wilkins E, Wilson L, Wickramasinghe K et al. European Cardiovascular Disease Statistics 2017. Brussels: European Heart Network, 2017. Available from: https://www.bhf.org.uk/publications/statistics/european-cardiovascular-disease-statistics-2017
2. Chow CK, Jolly S, Rao-Melacini P, Fox KA, Anand SS, Yusuf S. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation 2010;121:750–8. https://doi.org/10.1161/CIRCULATIONAHA.109.891523
3. Perk J, De Backer G, Gohlke H et al. European Guidelines on Cardiovascular Disease Prevention in Clinical Practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). G Ital Cardiol (Rome) 2013;14:328–92. https://doi.org/10.1714/1264.13964
4. Barzi F, Woodward M, Marfisi RM, Tavazzi L, Valagussa F, Marchioli R. Mediterranean diet and all-causes mortality after myocardial infarction: results from the GISSI-Prevenzione trial. Eur J Clin Nutr 2003;57:604–11. https://doi.org/10.1038/sj.ejcn.1601575
5. Houston TK, Allison JJ, Person S, Kovac S, Williams OD, Kiefe CI. Post-myocardial infarction smoking cessation counseling: associations with immediate and late mortality in older Medicare patients. Am J Med 2005;118:269–75. https://doi.org/10.1016/j.amjmed.2004.12.007
6. Trichopoulou A, Bamia C, Norat T et al. Modified Mediterranean diet and survival after myocardial infarction: the EPIC-Elderly study. Eur J Epidemiol 2007;22:871–81. https://doi.org/10.1007/s10654-007-9190-6
7. National Statistics Office, Malta. Demographic review 2010. Valletta: National Statistics Office, 2011. Available from: https://nso.gov.mt/en/publicatons/Pages/Publications-by-Date.aspx
8. Kotseva K, Wood D, De Backer G, De Backer D, Pyorala K, Keil U. Cardiovascular prevention guidelines in daily practice: a comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet 2009;373:929–40. https://doi.org/10.1016/S0140-6736(09)60330-5
9. Teo K, Lear S, Islam S et al. Prevalence of a healthy lifestyle among individuals with cardiovascular disease in high-, middle- and low-income countries: the Prospective Urban Rural Epidemiology (PURE) study. JAMA 2013;309:1613–21. https://doi.org/10.1001/jama.2013.3519
10. Jorenby DE, Hays JT, Rigotti NA et al. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA 2006;296:56–63. https://doi.org/10.1001/jama.296.1.56
11. Molyneux A, Lewis S, Leivers U et al. Clinical trial comparing nicotine replacement therapy (NRT) plus brief counselling, brief counselling alone, and minimal intervention on smoking cessation in hospital inpatients. Thorax 2003;58:484–8. https://doi.org/10.1136/thorax.58.6.484
12. Rovina N, Nikoloutsou I, Katsani G et al. Effectiveness of pharmacotherapy and behavioral interventions for smoking cessation in actual clinical practice. Ther Adv Respir Dis 2009;6:279–87. https://doi.org/10.1177/1753465809350653
13. Stead LF, Perera R, Bullen C et al. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev 2012;11:CD000146. https://doi.org/10.1002/14651858.CD000146.pub4
14. DeBoer SW, Thomas RJ, Brekke MJ et al. Dietary intake of fruits, vegetables, and fat in Olmsted County, Minnesota. Mayo Clin Proc 2003;78:161–6. https://doi.org/10.4065/78.2.161
15. Vannoni F, Spadea T, Frasca G et al. Association between social class and food consumption in the Italian EPIC population. Tumori 2003;89:669–78.
16. Meier C, Ackermann-Liebrich U. Socioeconomic class as a risk factor for cardiovascular diseases. Ther Umsch 2005;62:591–5. https://doi.org/10.1024/0040-5930.62.9.591
17. Westerterp KR, Meijer EP. Physical activity and parameters of aging: a physiological perspective. J Gerontol A Biol Sci Med Sci 2001;56:7–12. https://doi.org/10.1093/gerona/56.suppl_2.7
18. Dimatteo MR, Haskard KB, Williams SL. Health beliefs, disease severity, and patient adherence: a meta-analysis. Med Care 2007;45:521–8. https://doi.org/10.1097/MLR.0b013e318032937e
19. Salmon J, Owen N, Crawford D, Bauman A, Sallis JF. Physical activity and sedentary 22:178–88. https://doi.org/10.1037/0278-6133.22.2.178
20. Rimmer JH, Nicola T, Riley B, Creviston T. Exercise training for African Americans with disabilities residing in difficult social environments. Am J Prev Med 2002;23:290–5. https://doi.org/10.1016/S0749-3797(02)00517-2
21. Fry J, Finley W. The prevalence and costs of obesity in the EU. Proc Nutr Soc 2005;64:359–62. https://doi.org/10.1079/PNS2005443
22. Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med 2000;160:3278–85. https://doi.org/10.1001/archinte.160.21.3278
23. Ryden L, Standl E, Bartnik M et al. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J 2007;28:88–136. https://doi.org/10.1093/eurheartj/ehl260
24. Dullaghan L, Lusk L, McGeough M, Donnelly P, Herity N, Fitzsimons D. ‘I am still a bit unsure how much of a heart attack it really was!’ Patients presenting with non ST elevation myocardial infarction lack understanding about their illness and have less motivation for secondary prevention. Eur J Cardiovasc Nurs 2014;13:270–6. https://doi.org/10.1177/1474515113491649
25. Strid C, Lingfors H, Fridlund B, Martensson J. Lifestyle changes in coronary heart disease: effects of cardiac rehabilitation programs with focus on intensity, duration and content. A systematic review. Open Journal of Nurs 2016;2:420–30. https://doi.org/10.4236/ojn.2012.24060
