The clinical presentation of patients with cardiac tamponade largely depends upon the length of time over which pericardial fluid accumulates and the clinical situation. It can result in a clinical picture ranging from cardiogenic shock to general malaise, including dyspnoea, chest discomfort or fullness, peripheral oedema and fatiguability.
Although cardiac tamponade is a clinical diagnosis, two-dimensional and Doppler echocardiography play major roles in the identification of pericardial effusion and in assessing its haemodynamic significance. Despite this, some other imaging techniques or diagnostic tools could also be used for diagnosis. With this case we want to highlight not only the role of the electrocardiogram (ECG), but also its utility in assessing the haemodynamic changes in this clinical entity.
Case report
A 72-year-old man was admitted to our hospital for asthenia and general malaise for a week. He had a history of alcoholism, hypertension, diabetes, dyslipidaemia and peripheral artery disease with stent implantation in both iliac arteries.
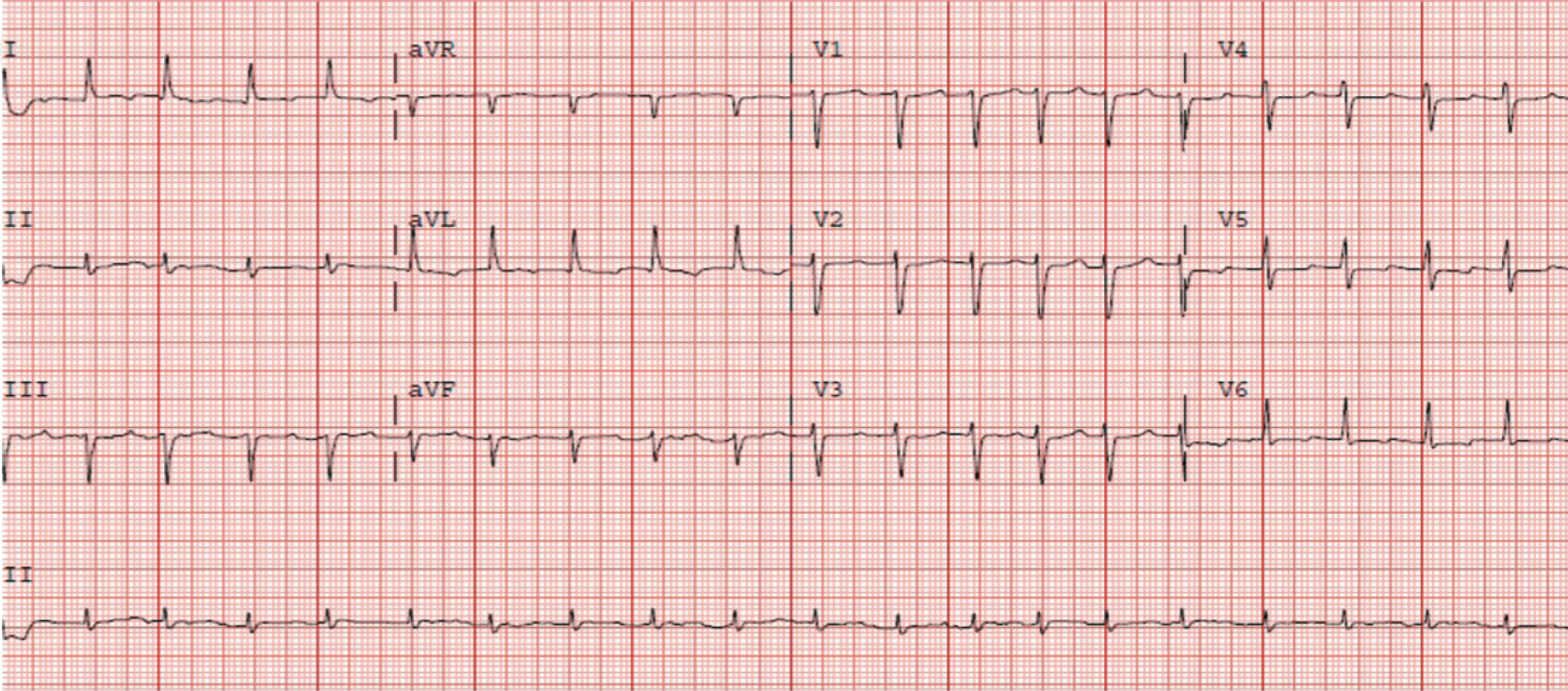
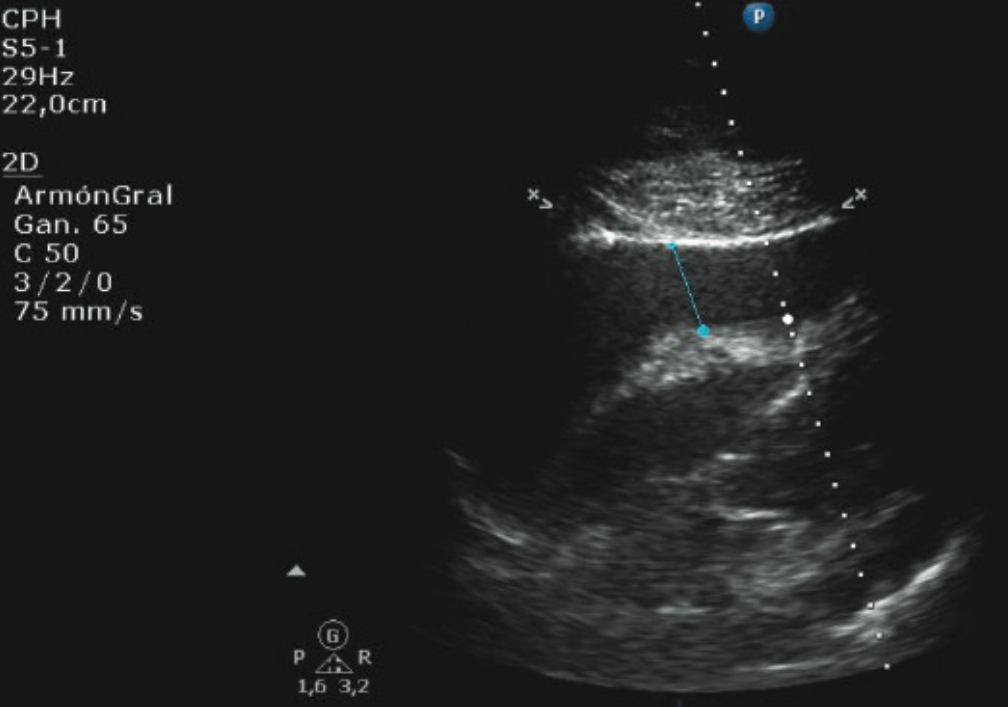
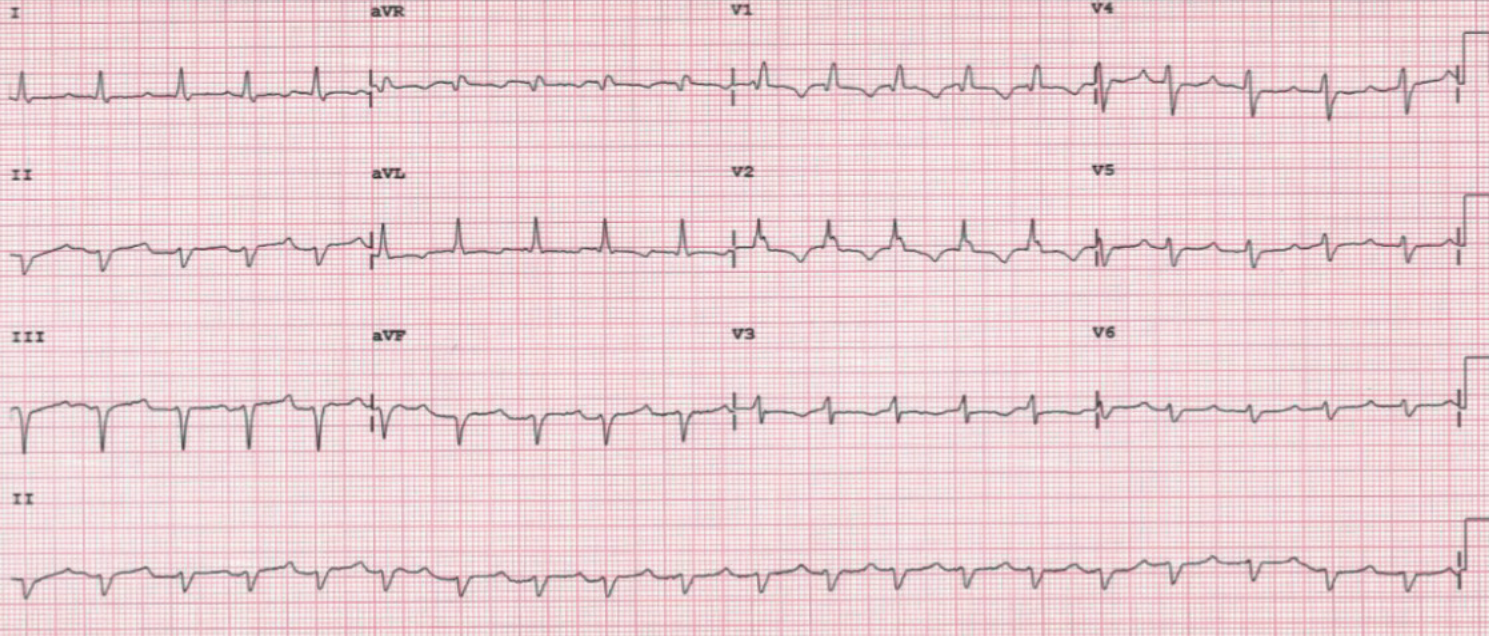
Five days before, he was admitted to the emergency department for asthenia and was diagnosed with atrial fibrillation and secondary congestive heart failure. Therapy with enoxaparin and warfarin was initiated, added to his long-term treatment with aspirin, but his symptoms worsened. On arrival, an ECG was performed showing sinus tachycardia with a narrow QRS complex (figure 1). Echocardiography showed a severe pericardial effusion (figure 2) with signs of cardiac tamponade. A thoraco-abdominal computed tomography (CT) scan was performed with no evidence of aortic dissection or pulmonary thromboembolism. Consequently, an urgent pericardiocentesis was carried out with extraction of 600 ml of haemorrhagic fluid. After the procedure the ECG was repeated, showing the same sinus tachycardia but with widened QRS due to new-onset right bundle branch block (figure 3).
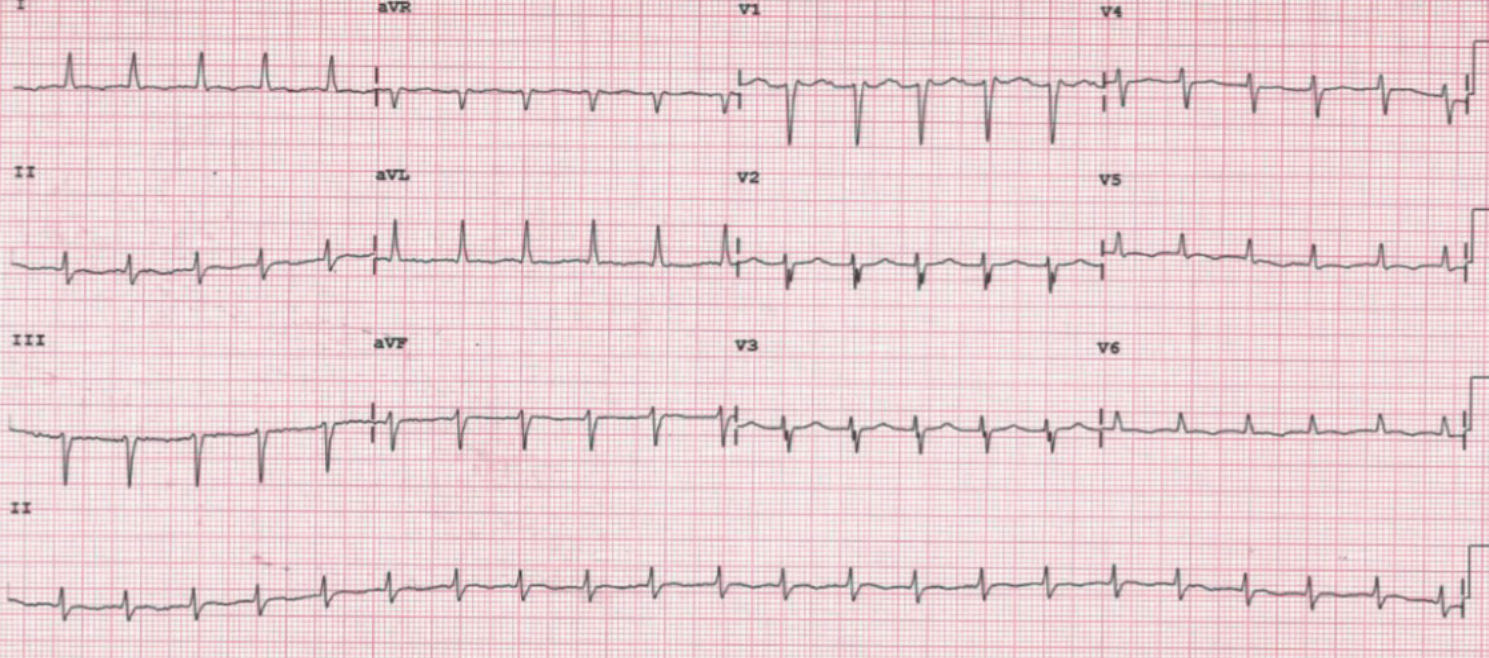
The patient recovered progressively during the following days, with haemodynamic stability and analytical improvement (including lactic acid, renal and hepatic functions). After extensive thorough evaluation, triple therapy with aspirin, enoxaparin and warfarin was the only explanation for the haemorrhagic fluid. Follow-up echocardiogram showed severe biventricular dysfunction without segmental anomalies; 24 hours later, the ECG was again narrow and similar to the admission ECG (figure 4).
Discussion
Right bundle branch block (RBBB) is a common expression of cor pulmonale, myocardial ischaemia/infarction, pulmonary embolism, myocarditis, or congenital heart disease; all of these involve right-side heart affection. Moreover, it is also known that the prevalence of RBBB increases with age and hypertension and is higher in men and diabetic patients. It has been associated with an adverse prognosis in patients with heart failure.1
Potential aetiologies for new-onset RBBB include:
- Acute pulmonary thromboembolism with right heart overload. This first one was probable in this case, but was excluded with the CT scan.
- Myocardial ischaemia secondary to coronary atherosclerotic affection or due to damage during the pericardiocentesis: this option was not probable due to normal cardiac troponin values and no other changes in ECG.
- Electrolyte abnormalities such as hyperkalaemia or even hypothermia were also ruled out.
- Rate-dependant phase 3 branch block was not possible due to the fact that the heart rate was higher earlier with a narrow complex.
- Drugs that could broaden the QRS complex, such as type I anti-arrhythmic drugs and related sodium-channel blocking agents (e.g. tricyclic antidepressants and phenothiazines).
Our hypothesis is that, although not described yet, a fast decompression of pericardial effusion could generate an acute right heart overload and a transient RBBB, as well as the more common right heart failure ex vacuum.2-4 In the same way that the well-known association between acute pulmonary thromboembolism and a new RBBB due to an acute right heart overload, it is known that after pericardiocentesis a substantial increase in right ventricular filling pressure occurs. The most well-known ECG readings in cardiac tamponade are low QRS voltages and electrical alternans and T-wave inversion, but we did not find these in this case.5
Conclusion
The haemodynamic changes observed during pericardial effusion/cardiac tamponade can be represented through the surface ECG. The volume overload on the right ventricle after a fast decompression of pericardial space due to pericardiocentesis can result in right His-bundle branch block.
This well-known relationship between haemodynamic changes and ECG in other entities, such as acute pulmonary embolism, can also be applied to cardiac tamponade.
Conflict of interest
None declared.
Key messages
- The haemodynamic changes that occur during a cardiac tamponade can be reflected in the surface electrocardiogram (ECG)
- After a pericardiocentesis the right ventricle volume overload can cause a right bundle branch block
References
1. Bussink BE, Holst AG, Jespersen L, Deckers JW, Jensen GB, Prescott E. Right bundle branch block: prevalence, risk factors, and outcome in the general population: results from the Copenhagen City Heart Study. Eur Heart J 2013;34:138–46. https://doi.org/10.1093/eurheartj/ehs291
2. Ligero C, Leta R, Bayes-Genis A. Transient biventricular dysfunction following pericardiocentesis. Eur J Heart Fail 2006;8:102–4. https://doi.org/10.1016/j.ejheart.2005.05.012
3. Ditchey R, Engler R, LeWinter M et al. The role of the right heart in acute cardiac tamponade in dogs. Circ Res 1981;48:701–10. https://doi.org/10.1161/01.RES.48.5.701
4. Reddy PS, Curtiss EI, Uretsky BF. Spectrum of hemodynamic changes in cardiac tamponade. Am J Cardiol 1990;66:1487–91. https://doi.org/10.1016/0002-9149(90)90540-H
5. Friedman HS, Gomes JA, Tardio AR, Haft JI. The electrocardiographic features of acute cardiac tamponade. Circulation 1974;50:260–5. https://doi.org/10.1161/01.CIR.50.2.260
