Inflammation plays an important role in the pathogenesis of coronary heart disease (CHD). Several inflammatory cytokines have shown a direct association with the development of atherosclerosis. Recently, there have been a number of experimental studies exploring the potential anti-inflammatory role of currently used therapeutic agents including antibiotics, immuno-suppressive drugs and non-steroidal anti-inflammatory medications. This review summarises the available evidence base and the potential role of these agents in current clinical practice.
Introduction
Coronary heart disease (CHD) is the leading cause of death worldwide. Chronic subclinical inflammation is a key recognised process in the pathogenesis of CHD, and may play an important role in atherogenesis.

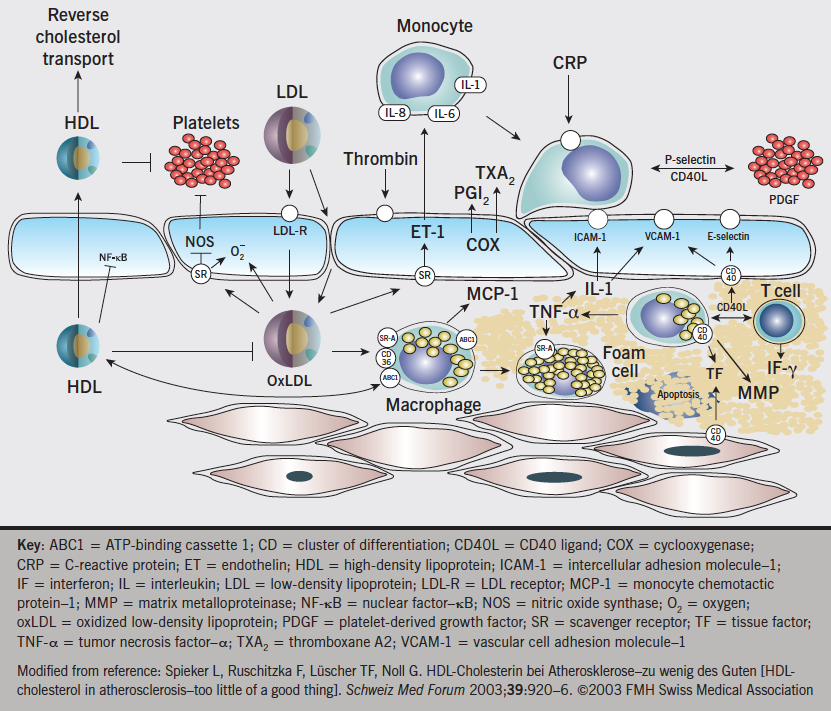
Atherosclerosis is a complex multi-factorial disease process, which is initiated at the endothelium in response to various forms of injurious stimuli (shear stress, oxidative stress, arterial pressure changes) including inflammation. These factors appear to alter the endothelial cell’s capacity to maintain homeostasis and vascular tone and leads to the so-called endothelial ‘dysfunction’, predisposing to the development of atherosclerosis. Inflammation appears to act as a significant trigger in the atherosclerotic plaque rupture (see figure 1), preceding acute cardiac events.
Inflammation and atherosclerosis
The degree of inflammatory activity, as detectable both within the atherosclerotic plaque and in the circulation, is associated with plaque destabilisation and atherothrombotic complications. It has become apparent that both endothelial cell activation and monocyte/macrophage activation play a significant role in rapid coronary artery disease (CAD) progression. Endothelial cell activation is accompanied by the enhanced expression of cell adhesion molecules, such as vascular cell adhesion molecule-1 (VCAM-1), a significant reduction in nitric oxide production, and a remarkable increase in the formation of reactive oxygen species. As a result, endothelial function is impaired, and the inflammatory cascade is activated with release of cytokines and growth factors. These factors stimulate migration and proliferation of vascular smooth muscle cells and fibroblasts, which form a fibrous cap over the atherosclerotic lesion.
Interleukin-6 (IL-6) an inflammatory cytokine produced mainly by T cells, macrophages, and adipocytes, promotes inflammatory responses via the membrane-bound or circulating soluble interleukin-6 receptor (IL-6R) on monocytes, hepatocytes, and endothelial cells. High-circulating concentrations of IL-6 are associated with increased risk of CHD events in prospective observational studies. Subsequently, the cap becomes weak, following release of proteolytic enzymes, leading to plaque rupture and exposure of underlying collagen to platelets, and subsequent thrombus formation, which can result in acute coronary syndrome.
Inflammation has also been extended to the disorders of coronary microvasculature, and associated with special subsets of CAD, such as silent myocardial ischaemia, myocardial ischaemia–reperfusion, cardiac syndrome X, variant angina, coronary artery ectasia, coronary calcification and in-stent restenosis.
Several systemic inflammatory markers reflect different degrees of inflammation and have been implicated as independent risk factors in cardiovascular disease, especially in unstable coronary syndromes. A series of prospective studies provide consistent data documenting that mild elevation of baseline levels of high-sensitivity C-reactive protein (hs-CRP) among apparently healthy individuals is associated with higher long-term risk for cardiovascular events. Recent studies suggest that, besides CRP, other inflammatory biomarkers such as cytokines (interleukin [IL]-1, IL-6, IL-8, monocyte chemo-attractant protein-1 [MCP-1]), soluble CD40 ligand, serum amyloid A (SAA), selectins (E-selectin, P-selectin), myeloperoxidase (MPO), matrix metalloproteinase (MMPs), cellular adhesion molecules (intercellular adhesion molecule 1 [ICAM-1], VCAM-1), placental growth factor (PlGF) and A(2) phospholipases may have a potential role for the prediction of risk for rapid progression of CAD, regardless of plaque morphology (figure 2).
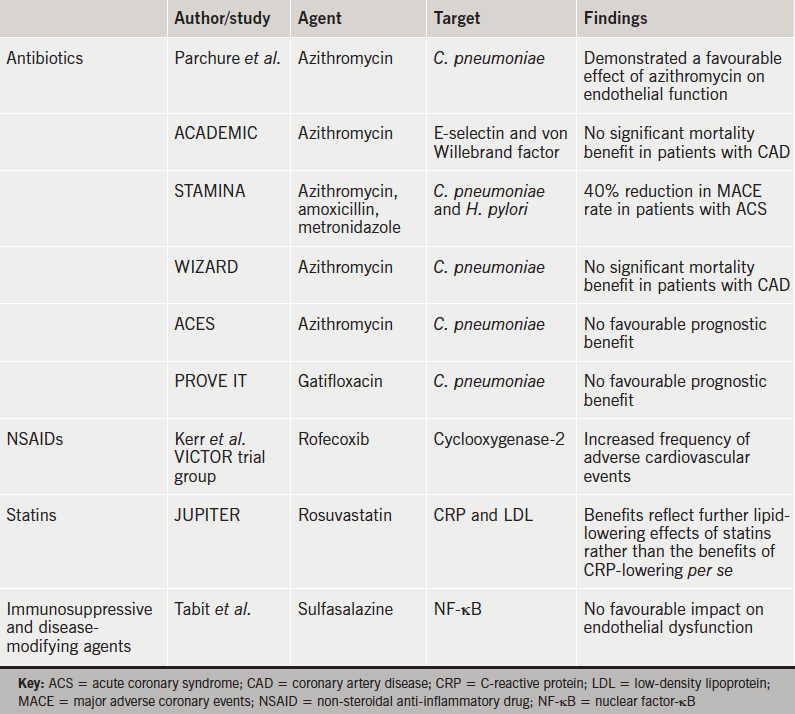
It is less clear, however, whether elevated levels of circulating inflammatory markers play a role in the extent and severity of atherosclerosis, and such pathobiological paradigms remain controversial. The identification of inflammatory biomarkers and cellular/molecular pathways in atherosclerotic disease represent important goals in cardiovascular disease research, in particular, with respect of the development of therapeutic strategies to prevent or reverse atherosclerotic diseases. This pathophysiology is amenable to modification by drugs targeting cell proliferation, cell migration, osteogenic/fibrous turnover of the extracellular matrix ranging from anti-metabolites, glucocorticoids, specific cytokine and leukotriene antagonists to classic immunosuppressive agents and vaccines directed specifically at certain relevant diseases (table 1).
Antibiotics
Recently, there have been a number of experimental studies exploring the potential anti-inflammatory role of currently used therapeutic agents. Sulfasalazine is a disease-modifying agent which acts as an inhibitor of nuclear factor-κB (NF-κB). In experimental studies, NF-κB acts as an inflammatory regulator and is known to cause endothelial cell dysfunction and reduce nitric oxide production. However, in a recent study by Tabit et al., the clinical use of sulfasalazine in patients with established CAD, was not demonstrated to have any favourable impact on improvement of endothelial dysfunction.1
Antibiotics may play a role in the general inflammatory process, possibly by down-regulating pro-inflammatory cytokines. Parchure et al., demonstrated a favourable effect of azithromycin on endothelial function in patients with Chlamydophila pneumoniae infection with known CAD.2 This was also evident in the ACADEMIC (Azithromycin in Coronary Artery Disease: Elimination of Myocardial Infection with Chlamydia) study where the levels of E-selectin and von Willebrand factor were significantly reduced in the treatment arm. However, despite this effect, azithromycin failed to show any significant mortality benefit in patients with CAD.3 In contrast, the STAMINA (South Thames Trial of Antibiotics in Myocardial Infarction and Unstable Angina) trial reported a 40% reduction in major cardiac event rate in patients with acute coronary syndromes (ACS) who received the same antibiotic treatment during hospital admissions.4 The reason for these contradictory findings remains unexplained.
The WIZARD (Weekly Intervention with Zithromax for Atherosclerosis and its Related Disorders) study was a randomised-controlled trial, which aimed to understand the impact of antibiotics on CAD events. Similar to the ACADEMIC trial, this study also failed to show any evidence for reduction of cardiac events in stable post-myocardial infarction patients, who were treated with azithromycin following exposure to C. pneumoniae.5 Another, the ACES (Azithromycin and Coronary Events Study) trial, was one of the largest randomised, placebo-controlled trials, in which more than 2,000 patients were randomised to receive azithromycin or placebo, with a follow-up of four years. Despite confirming the presence of C. pneumonia in atherosclerotic plaque lesions, azithromycin therapy was not associated with any favourable prognostic benefit.6
A new generation of antibiotic, fluoroquinolone gatifloxacin, was also found to be less effective in reducing cardiac events in the recent PROVE IT (Pravastatin or Atorvastatin Evaluation and Infection Therapy) trial.7 The results of these trials affirm and strengthen the recommendation against prophylactic use of antibiotics to prevent future cardiac events among people with established CAD.
Fibrinogen
The presence of elevated fibrinogen levels in blood is also indicative of active inflammatory processes. In epidemiological studies, increased fibrinogen levels have been shown to be associated with risk of developing ischaemic heart disease. However, it is not apparent whether this association reflects causation, in the context of the simultaneous presence of other risk factors. In a recent meta-analysis by Danesh et al., a putative link between serum fibrinogen levels and CHD has been demonstrated.8 However, Keavney et al. proved, using genetically based analyses, that there is no major association between fibrinogen level and risk of CAD.9
Non-steroidal anti-inflammatory drugs
Anti-inflammatory compounds include cyclooxygenase-2 inhibitors and other inhibitors of eicosanoid synthesis. An increased incidence of cardiovascular events in patients treated with the cyclooxygenase-2 inhibitor rofecoxib indicates the need for a cautious approach with these medications in patients with cardiovascular disease.10 Aspirin is an antiplatelet and anti-inflammatory drug. It acts by down-regulating eicosanoid synthesis, and the benefits of reducing risk of first myocardial infarction are maximised in patients with inflammation and elevated CRP levels. Low-dose aspirin has antiplatelet effects, stabilises atherosclerotic plaques, and reduces inflammation in coronary vessels.
Statins and role of CRP
Statins are a very effective group of medications for primary and secondary prevention of atherosclerotic disease, which act by reducing low-density lipoprotein (LDL)-cholesterol levels, as well as by reducing CRP levels with an additional anti-inflammatory effect. There is a direct correlation between statin therapy and lower CRP concentrations, as shown in several studies and trials. They prevent recruitment, migration and cell adhesion to endothelium by lowering cytokine concentrations and reducing chemokine production. In addition, they increase the production of nitric oxide, and hence, protect the endothelium. They also inhibit inflammatory pathways regulated by proteins such as Ras and Rho.11
The recommendation for statin therapy in otherwise healthy individuals with low levels of LDL and high levels of CRP is controversial. JUPITER (Justification for the Use of Statins in Primary Prevention: An Intervention Trial Evaluating Rosuvastatin trial),12 a major randomised, double-blind, placebo-controlled trial, was designed to investigate the use of rosuvastatin in the primary prevention of cardiovascular disease. This was focused on patients with normal LDL-cholesterol levels but increased levels of hsCRP, and the results demonstrated that the benefits in this group of patients may simply reflect further lipid-lowering effects in people who would not be considered for pharmacotherapy, rather than the benefits of CRP-lowering per se. Ridker et al.12 did not support the development of therapeutic strategies specific for lowering CRP levels in plasma in this study.
In 2009, the Mendelian randomisation study published in the Journal of the American Medical Association suggested that CRP does not play a causal role in cardiovascular disease. However, it still could be a useful marker of cardiovascular disease risk.13 This provoked a debate over the role and value of CRP as a biomarker and possible therapeutic target in heart disease. Moreover, in their British Medical Journal article in 2011, the C-Reactive Protein Coronary Heart Disease Genetics Collaboration (CCGC) suggested that CRP level is unlikely to be even a modest causal factor in CHD.14
Other therapies
The immunosuppressive drugs cyclosporine and sirolimus block the activation of T cells and prevent smooth-muscle proliferation. Sirolimus-coated stents are currently used to prevent restenosis after angioplasty. It is not yet known whether or not this family of compounds can be used in ACS.
Therapies based on elevating levels of high-density lipoprotein (HDL) have the potential for acting through the attenuation of acute and chronic conditions of inflammation as they relate to atherosclerosis. HDL itself, for example, may have inhibitory effects on the activation of macrophages and other immune cells promoting healthy endothelial function and inhibiting the formation of atherosclerosis. Recent studies suggest that HDL inhibits growth factors and cytokine receptor signalling, and may also participate in reverse cholesterol transport. Conversely, circulating dysfunctional HDLs are associated with inflammation due to their pro-oxidative and pro-inflammatory properties.15
Cyclosporine A is a potent inhibitor of the myocardial cell mitochondrial permeability transition pore (MPTP). The opening of the MPTP at the time of myocardial reperfusion following percutaneous coronary intervention or thrombolysis could trigger metabolic alterations and release of cytokines leading to cardiomyocyte death. A pilot study by Piot et al16 indicated that administration of cyclosporine at the time of reperfusion was associated with a reduction in the infarct size in STEMI, limiting the impact of ischaemic-reperfusion related cell injury. This work has been substantiated by Mewton et al.17 in a follow up study, which demonstrated sustained improved left ventricular function with no evidence of adverse remodelling. The ongoing CIRCUS18 trial (Cyclosporine to ImpRove Clinical oUtcome in ST-elevation myocardial infarction patients) is likely to consolidate the evidence to support the potential clinical utility of cyclosporine A in acute STEMIs. Other cyclosporins may also prove to be of potential value.
Biomarkers such as IL-6 and soluble interleukin-6 receptor (sIL-6R) are elevated in acute myocardial infarction. A Mendelian randomisation analysis in The Lancet, 2012, reported that there is robust genetic evidence for the role of a specific inflammatory pathway in the development of CHD in humans. A variant in the IL-6R gene had effects on biomarkers of inflammation and related inflammatory pathways. There is strong evidence of IL-6R signalling in the development of CHD. The specific Mendelian randomisation analyses for IL-6 have not been done yet. However, more randomised trials are required to test these more novel therapeutic approaches of IL-6R blockade in preventing CAD.19
There have been a number of phase III trials of various anti-inflammatory agents to test their effectiveness in the secondary prevention of cardiovascular disease, including two trials of darapladib (an inhibitor of lipoprotein-associated phospholipase A2),20 a trial of canakinumab (a monoclonal antibody to interleukin 1β),21 and a trial of low-dose methotrexate.22
The secretory phospholipase inhibitors, e.g. varespladib (a non-specific sPLA2 inhibitor) or darapladib (a targeted LpPLA2 inhibitor) are effective agents for reducing sPLA2 and Lp-PLA2, respectively, but do not have a significant effect on the central IL-6 regulatory pathway and CRP, as evidenced by the FRANCIS (Fewer Recurrent Acute coronary events with Near-term Cardiovascular Inflammation Suppression) trial and in PLASMA (Phospholipase Levels and Serological Markers of Atherosclerosis) studies in the varespladib group. Similarly, in the Integrated Biomarker and Imaging Study (IBIS-2), it was observed that darapladib does not have effect on primary end points of CRP level or coronary atheroma deformability. However, improvement in progression of lipid necrotic core was noticed.23
In their 2013 study, Anderson et al. suggest that in ACS, the pathogenesis of unstable plaque and rupture can be explained by changes in intracellular signalling with trans-IL-6 receptor binding and by blocking of IL-6 receptors.24
Conclusion
In conclusion, multiple factors, including inflammation, are responsible for the complex pathogenesis of atherosclerosis in coronary arteries. Rapid CAD progression is associated with endothelial and macrophage/monocyte activation, release of cytokines and elevated inflammatory markers, but their effect on the extent and severity of atherosclerosis remains controversial. However, they play an important role in cardiovascular research on the development of therapeutic strategy.
The use of some anti-inflammatory compounds is associated with increased cardiovascular events and requires a cautious approach. Antibiotics may have some role in down-regulating inflammatory processes, but there is no definite evidence of prophylactic antibiotics preventing cardiac events. Statins have an additional anti-inflammatory effect through reducing CRP levels, but are not recommended in patients with normal cholesterol and high hsCRP levels because CRP does not play a causal role in cardiovascular disease. The benefits of statins are related to further lowering of cholesterol levels, rather than an anti-inflammatory effect. Systemic use of immunosuppressive medications has significant side effects; however, localised effects with sirolimus-coated stents can be used to prevent restenosis.
The HDL-based therapy is promising and likely to have an inhibitory effect on the inflammatory cascade, and, hence, reduce atherosclerosis. However, further evidence is needed because dysfunctional HDL particles in blood are harmful due to their pro-inflammatory effect. Recently, a few prospective studies have shown that levels of circulating IL-6 and sIL-6R are elevated in ACS patients and are associated with increased risk of CHD. This has been confirmed with strong genetic evidence in a Mendelian randomisation study, and IL-6R blockade could develop a new therapeutic approach in future, which would require multiple randomised trials before its implication in clinical practice.
Conflict of interest
None declared.
Key messages
- Inflammation plays a significant role in the pathogenesis of atherosclerosis and coronary artery disease progression
- Many currently used therapeutic agents (antibiotics, immunosuppressive agents, statins) seem to have an impact on down-regulating the inflammatory process associated with atherosclerotic coronary artery disease but with no significant beneficial impact on reducing cardiovascular events
- Future studies are needed to establish the potential clinical utility of these novel compounds to treat and prevent coronary heart disease
- We appear to be no nearer attenuating a potentially adverse core mechanism in the natural history of myocardial infarction. This is an important area for future translational research
References
1. Tabit CE, Holbrook M, Shenouda SM et al. Effect of sulfasalazine on inflammation and endothelial function in patients with established coronary artery disease. Vasc Med 2012;17:101–07. http://dx.doi.org/10.1177/ 1358863X12440117
2. Parchure N, Zouridakis EG, Kaski JC. Effect of azithromycin treatment on endothelial function in patients with coronary artery disease and evidence of chlamydia pneumoniae infection. Circulation 2002;105:1298–303. http://dx.doi.org/10.1161/hc1102.105649
3. Anderson JL, Muhlestein JB. The ACADEMIC study in perspective (Azithromycin in coronary artery disease: elimination of myocardial infection with Chlamydia). J Infect Dis 2000;181:S569–S571. http://dx.doi.org/10.1086/315635
4. Stone AF, Mendall MA, Kaski JC et al. Effect of treatment for Chlamydia pneumoniae and Helicobacter pylori on markers of inflammation and cardiac events in patients with acute coronary syndromes: South Thames Trial of Antibiotics in Myocardial Infarction and Unstable Angina (STAMINA). Circulation 2002;106:1219–23. http://dx.doi.org/10.1161/01.CIR.0000027820.66786.CF
5. O’Connor CM, Dunne MW, Pfeffer MA et al.; Investigators in the WIZARD Study. Azithromycin for the secondary prevention of coronary heart disease events: the WIZARD study: a randomized controlled trial. JAMA 2003;290:1459–66. http://dx.doi.org/10.1001/jama.290.11.1459
6. Grayston JT, Kronmal RA, Jackson LA et al. Azithromycin for the Secondary Prevention of Coronary Events (ACES). N Engl J Med 2005;352:1637–45. http://dx.doi.org/10.1056/NEJMoa043526
7. Cannon CP, Braunwald E, McCabe CH et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 2004;350:1495–504. http://dx.doi.org/10.1056/NEJMoa040583
8. Danesh J, Lewington S, Thompson SG et al. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA 2005;294:1799–809. http://dx.doi.org/10.1001/jama.294.14.1799
9. Keavney B, Danesh J, Parish S et al. Fibrinogen and coronary heart disease: test of causality by ‘Mendelian randomization’. Int J Epidemiol 2006;35:935–43. http://dx.doi.org/10.1093/ije/dyl114
10. Kerr DJ, Dunn JA, Langman MJ et al. Rofecoxib and cardiovascular adverse events in adjuvant treatment of colorectal cancer. N Engl J Med 2007;357:360–9. http://dx.doi.org/10.1056/NEJMoa071841
11. Biasucci LM, Biasillo G, Stefanelli A. Inflammatory markers, cholesterol and statins: pathophysiological role and clinical importance. Clin Chem Lab Med 2010;48:1685–91. http://dx.doi.org/10.1515/CCLM.2010.277
12. Ridker P, Danielson E, Fonseca FAH, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008;359:2195–207. http://dx.doi.org/10.1056/NEJMoa0807646
13. Elliott P, Chambers JC, Zhang W et al. Genetic loci associated with C-reactive protein levels and risk of coronary heart disease. JAMA 2009;302:37–48. http://dx.doi.org/10.1001/jama.2009.954
14. Wensley F, Gao P, Burgess S et al. Association between C reactive protein and coronary heart disease: Mendelian randomization analysis based on individual participant data. BMJ 2011;342:d548. http://dx.doi.org/10.1136/bmj.d548
15. Haas MJ, Mooradian AD. Inflammation, high-density lipoprotein and cardiovascular dysfunction. Curr Opin Infect Dis 2011;24:265–72. http://dx.doi.org/10.1097/QCO.0b013e328344b724
16. Piot C, Croisille P, Staat P, et al. Effect of cyclosporine on reperfusion injury in acute myocardial infarction. N Engl J Med 2008;359:473–81. http://dx.doi.org/10.1056/NEJMoa071142
17. Mewton N, Croisille P, Gahide G, et al. Effect of cyclosporine on left ventricular remodeling after reperfused myocardial infarction. J Am Coll Cardiol 2010;55:1200–5. http://dx.doi.org/10.1016/j.jacc.2009.10.052
18. Mewton N, Cung TT, Morel O, et al. Rationale and design of the Cyclosporine to ImpRove Clinical oUtcome in ST-elevation myocardial infarction patients (the CIRCUS trial). Am Heart J 2015;169:758–66. http://dx.doi.org/10.1016/j.ahj.2015.02.020
19. The Interleukin-6 Receptor Mendelian Randomisation Analysis (IL6R MR) Consortium. The interleukin-6 receptor as a target for prevention of coronary heart disease: a Mendelian randomisation analysis. Lancet 2012;379:1214–24. http://dx.doi.org/10.1016/S0140-6736(12)60110-X
20. Lp-PLA2 Studies Collaboration. Lipoprotein-associated phospholipase A2 and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet 2010;375:1536–44. http://dx.doi.org/10.1016/S0140-6736(10)60319-4
21. Ridker PM, Thuren T, Zalewski A, Libby P. Interleukin-1β inhibition and the prevention of recurrent cardiovascular events: rationale and design of the Canakinumab Anti-inflammatory Thrombosis Outcomes Study (CANTOS). Am Heart J 2011;162:597–605. http://dx.doi.org/10.1016/j.ahj.2011.06.012
22. Ridker PM. Testing the inflammatory hypothesis of atherothrombosis: scientific rationale for the cardiovascular inflammation reduction trial (CIRT). J Thromb Haemost 2009;7:332–9. http://dx.doi.org/10.1111/j.1538-7836.2009.03404.x
23. Ridker PM, Lüscher TF. Anti-inflammatory therapies for cardiovascular disease. Eur Heart J 2014;35:1782–91. http://dx.doi.org/10.1093/eurheartj/ehu203
24. Anderson DR, Poterucha JT, Mikuls TR et al. IL-6 and its receptors in coronary artery disease and acute myocardial infarction. Cytokine 2013;62:395–400. http://dx.doi.org/10.1016/j.cyto.2013.03.020
